FDA Label for Cosentyx
View Indications, Usage & Precautions
- 1.1 PLAQUE PSORIASIS
- 1.2 PSORIATIC ARTHRITIS
- 1.3 ANKYLOSING SPONDYLITIS
- 1.4 NON-RADIOGRAPHIC AXIAL SPONDYLOARTHRITIS
- 2.1 TESTING AND PROCEDURES PRIOR TO TREATMENT INITIATION
- 2.2 PLAQUE PSORIASIS
- 2.3 PSORIATIC ARTHRITIS
- 2.4 ANKYLOSING SPONDYLITIS
- 2.5 NON-RADIOGRAPHIC AXIAL SPONDYLOARTHRITIS
- 2.6 IMPORTANT ADMINISTRATION INSTRUCTIONS
- 2.7 PREPARATION FOR USE OF COSENTYX SENSOREADY® PEN AND PREFILLED SYRINGE
- 2.8 RECONSTITUTION AND PREPARATION OF COSENTYX LYOPHILIZED POWDER
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5.1 INFECTIONS
- 5.2 PRE-TREATMENT EVALUATION FOR TUBERCULOSIS
- 5.3 INFLAMMATORY BOWEL DISEASE
- 5.4 HYPERSENSITIVITY REACTIONS
- 5.5 RISK OF HYPERSENSITIVITY IN LATEX-SENSITIVE INDIVIDUALS
- 5.6 IMMUNIZATIONS
- 6 ADVERSE REACTIONS
- 6.1 CLINICAL TRIALS EXPERIENCE
- 6.2 IMMUNOGENICITY
- 7 DRUG INTERACTIONS
- 8.1 PREGNANCY
- 8.2 LACTATION
- 8.4 PEDIATRIC USE
- 8.5 GERIATRIC USE
- 10 OVERDOSAGE
- 11 DESCRIPTION
- 12.1 MECHANISM OF ACTION
- 12.2 PHARMACODYNAMICS
- 12.3 PHARMACOKINETICS
- 13.1 CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
- 14.1 ADULT PLAQUE PSORIASIS
- 14.2 PEDIATRIC PLAQUE PSORIASIS
- 14.3 PSORIATIC ARTHRITIS
- 14.4 ANKYLOSING SPONDYLITIS
- 14.5 NON-RADIOGRAPHIC AXIAL SPONDYLOARTHRITIS
- 16.1 HOW SUPPLIED
- 16.2 STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PRINCIPAL DISPLAY PANEL
Cosentyx Product Label
The following document was submitted to the FDA by the labeler of this product Novartis Pharmaceuticals Corporation. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
1.1 Plaque Psoriasis
COSENTYX® is indicated for the treatment of moderate to severe plaque psoriasis in patients 6 years and older who are candidates for systemic therapy or phototherapy.
1.2 Psoriatic Arthritis
COSENTYX is indicated for the treatment of adult patients with active psoriatic arthritis.
1.3 Ankylosing Spondylitis
COSENTYX is indicated for the treatment of adult patients with active ankylosing spondylitis.
1.4 Non-Radiographic Axial Spondyloarthritis
COSENTYX is indicated for the treatment of adult patients with active non-radiographic axial spondyloarthritis (nr-axSpA) with objective signs of inflammation.
2.1 Testing And Procedures Prior To Treatment Initiation
- Perform the following evaluations prior to COSENTYX initiation:
- Evaluate patients for tuberculosis (TB) infection. COSENTYX initiation is not recommended in patients with active TB infection. Initiate treatment of latent TB prior to initiation of COSENTYX [see Warnings and Precautions (5.2)].
- Complete all age-appropriate vaccinations as recommended by current immunization guidelines prior to initiating treatment with COSENTYX [see Warnings and Precautions (5.6)].
2.2 Plaque Psoriasis
Adults
The recommended dosage is 300 mg by subcutaneous injection at Weeks 0, 1, 2, 3, and 4 followed by 300 mg every 4 weeks. Each 300 mg dosage is given as 2 subcutaneous injections of 150 mg.
For some patients, a dose of 150 mg may be acceptable.
Pediatric Patients
The recommended dosage for pediatric patients 6 years of age and older is based on body weight (Table 1) and administered by subcutaneous injection at Weeks 0, 1, 2, 3, and 4 followed by dosing every 4 weeks.
| Body Weight at Time of Dosing | Recommended Dose |
| Less than 50 kg | 75 mg |
| Greater than or equal to 50 kg | 150 mg |
2.3 Psoriatic Arthritis
For psoriatic arthritis patients with coexistent moderate to severe plaque psoriasis, use the dosing and administration recommendations for plaque psoriasis [see Dosage and Administration (2.1)].
For other psoriatic arthritis patients, administer COSENTYX with or without a loading dosage by subcutaneous injection. The recommended dosage:
- With a loading dosage is 150 mg at Weeks 0, 1, 2, 3, and 4 and every 4 weeks thereafter
- Without a loading dosage is 150 mg every 4 weeks
- If a patient continues to have active psoriatic arthritis, consider a dosage of 300 mg every 4 weeks.
COSENTYX may be administered with or without methotrexate.
2.4 Ankylosing Spondylitis
Administer COSENTYX with or without a loading dosage by subcutaneous injection. The recommended dosage:
- With a loading dosage is 150 mg at Weeks 0, 1, 2, 3, and 4 and every 4 weeks thereafter
- Without a loading dosage is 150 mg every 4 weeks
- If a patient continues to have active ankylosing spondylitis, consider a dosage of 300 mg every 4 weeks.
2.5 Non-Radiographic Axial Spondyloarthritis
Administer COSENTYX with or without a loading dosage by subcutaneous injection. The recommended dosage:
- With a loading dosage is 150 mg at Weeks 0, 1, 2, 3, and 4 and every 4 weeks thereafter
- Without a loading dosage is 150 mg every 4 weeks.
2.6 Important Administration Instructions
There are four presentations for COSENTYX (i.e., Sensoready pen, prefilled syringes [150 mg/mL, 75 mg/0.5 mL], and lyophilized powder in vial for reconstitution). The COSENTYX “Instructions for Use” for each presentation contains more detailed instructions on the preparation and administration of COSENTYX [see Instructions for Use]. The lyophilized powder in vial for reconstitution is for healthcare provider use only.
COSENTYX is intended for use under the guidance and supervision of a physician.
Sensoready Pen
Adult patients may self-administer COSENTYX or be injected by a caregiver after proper training in subcutaneous injection technique using the Sensoready pen.
Pediatric patients should not self-administer COSENTYX using the Sensoready pen. An adult caregiver should prepare and inject COSENTYX after proper training in subcutaneous injection technique using the Sensoready pen.
Prefilled Syringe
Adult patients may self-administer COSENTYX or be injected by a caregiver after proper training in subcutaneous injection technique using the prefilled syringe.
Pediatric patients should not self-administer COSENTYX using the prefilled syringe. An adult caregiver should prepare and inject COSENTYX after proper training in subcutaneous injection technique using the prefilled syringe.
Administration Instructions
Administer each injection at a different anatomic location (such as upper arms, thighs, or any quadrant of abdomen) than the previous injection, and not into areas where the skin is tender, bruised, erythematous, indurated, or affected by psoriasis. Administration of COSENTYX in the upper, outer arm may be performed by a caregiver or healthcare provider.
2.7 Preparation For Use Of Cosentyx Sensoready® Pen And Prefilled Syringe
Before injection, remove COSENTYX Sensoready pen or COSENTYX prefilled syringe from the refrigerator and allow COSENTYX to reach room temperature (15 to 30 minutes) without removing the needle cap.
The removable cap of the COSENTYX Sensoready pen and the COSENTYX prefilled syringe contain natural rubber latex and should not be handled by latex-sensitive individuals [see Warnings and Precautions (5.5)].
Inspect COSENTYX visually for particulate matter and discoloration prior to administration. COSENTYX injection is a clear to slightly opalescent, colorless to slightly yellow solution. Do not use if the liquid contains visible particles, is discolored or cloudy. COSENTYX does not contain preservatives; therefore, administer the Sensoready pen or prefilled syringe within 1 hour after removal from the refrigerator. Discard any unused product remaining in the Sensoready pen or prefilled syringe.
2.8 Reconstitution And Preparation Of Cosentyx Lyophilized Powder
COSENTYX lyophilized powder should be prepared and reconstituted with Sterile Water for Injection by a trained healthcare provider using aseptic technique and without interruption. The preparation time from piercing the stopper until end of reconstitution on average takes 20 minutes and should not exceed 90 minutes.
a) Remove the vial of COSENTYX lyophilized powder from the refrigerator and allow to stand for 15 to 30 minutes to reach room temperature. Ensure the Sterile Water for Injection is at room temperature.
b) Slowly inject 1 mL of Sterile Water for Injection into the vial containing COSENTYX lyophilized powder and direct the stream of Sterile Water for Injection onto the lyophilized powder.
c) Tilt the vial at an angle of approximately 45 degrees and gently rotate between the fingertips for approximately 1 minute. Do not shake or invert the vial.
d) Allow the vial to stand for about 10 minutes at room temperature to allow for dissolution. Note that foaming may occur.
e) Tilt the vial at an angle of approximately 45 degrees and gently rotate between the fingertips for approximately 1 minute. Do not shake or invert the vial.
f) Allow the vial to stand undisturbed at room temperature for approximately 5 minutes. The reconstituted COSENTYX solution should be essentially free of visible particles, clear to opalescent, and colorless to slightly yellow. Do not use if the lyophilized powder has not fully dissolved or if the liquid contains visible particles, is cloudy or discolored.
g) Prepare the required number of vials (1 vial for the 150 mg dose or 2 vials for the 300 mg dose).
h) The COSENTYX reconstituted solution contains 150 mg of secukinumab in 1 mL of solution. After reconstitution, use the solution immediately or store in the refrigerator at 2°C to 8°C (36°F to 46°F) for up to 24 hours. Do not freeze.
i) If stored at 2°C to 8°C (36°F to 46°F), allow the reconstituted COSENTYX solution to reach room temperature (15 to 30 minutes) before administration. COSENTYX does not contain preservatives; therefore, administer within 1 hour after removal from 2°C to 8°C (36°F to 46°F) storage.
3 Dosage Forms And Strengths
- Injection: 150 mg/mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose Sensoready pen
- Injection: 150 mg/mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose prefilled syringe
- Injection: 75 mg/0.5 mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose prefilled syringe (for pediatric patients less than 50 kg)
- For injection: 150 mg white lyophilized powder in a single-dose vial for reconstitution (for healthcare professional use only)
4 Contraindications
COSENTYX is contraindicated in patients with a previous serious hypersensitivity reaction to secukinumab or to any of the excipients in COSENTYX. Cases of anaphylaxis have been reported during treatment with COSENTYX [see Warnings and Precautions (5.4)].
5.1 Infections
COSENTYX may increase the risk of infections. In clinical trials, a higher rate of infections was observed in COSENTYX treated subjects compared to placebo-treated subjects. In placebo-controlled clinical trials in subjects with moderate to severe plaque psoriasis, higher rates of common infections, such as nasopharyngitis (11.4% versus 8.6%), upper respiratory tract infection (2.5% versus 0.7%) and mucocutaneous infections with candida (1.2% versus 0.3%) were observed with COSENTYX compared with placebo. A similar increase in risk of infection was seen in placebo-controlled trials in subjects with psoriatic arthritis, ankylosing spondylitis and non-radiographic axial spondyloarthritis. The incidence of some types of infections appeared to be dose-dependent in clinical studies [see Adverse Reactions (6.1)]. In the postmarketing setting, serious and some fatal infections have been reported in patients receiving COSENTYX.
Exercise caution when considering the use of COSENTYX in patients with a chronic infection or a history of recurrent infection.
Instruct patients to seek medical advice if signs or symptoms suggestive of an infection occur. If a patient develops a serious infection, monitor the patient closely and discontinue COSENTYX until the infection resolves.
5.2 Pre-Treatment Evaluation For Tuberculosis
Evaluate patients for tuberculosis (TB) infection prior to initiating treatment with COSENTYX. Avoid administration of COSENTYX to patients with active TB infection. Initiate treatment of latent TB prior to administering COSENTYX. Consider anti-TB therapy prior to initiation of COSENTYX in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed. Monitor patients closely for signs and symptoms of active TB during and after treatment.
5.3 Inflammatory Bowel Disease
Caution should be used when prescribing COSENTYX to patients with inflammatory bowel disease. Exacerbations, in some cases serious, occurred in COSENTYX treated subjects during clinical trials in plaque psoriasis, psoriatic arthritis, ankylosing spondylitis and non-radiographic axial spondyloarthritis. In addition, new onset inflammatory bowel disease cases occurred in clinical trials with COSENTYX. In an exploratory trial in 59 subjects with active Crohn’s disease, there were trends toward greater disease activity and increased adverse events in the secukinumab group as compared to the placebo group. Patients who are treated with COSENTYX should be monitored for signs and symptoms of inflammatory bowel disease [see Adverse Reactions (6.1)].
5.4 Hypersensitivity Reactions
Anaphylaxis and cases of urticaria occurred in COSENTYX treated subjects in clinical trials. If an anaphylactic or other serious allergic reaction occurs, administration of COSENTYX should be discontinued immediately and appropriate therapy initiated [see Contraindications (4), Adverse Reactions (6.1)].
5.5 Risk Of Hypersensitivity In Latex-Sensitive Individuals
The removable caps of the COSENTYX Sensoready pen and the COSENTYX 1 mL and 0.5 mL prefilled syringes contain natural rubber latex, which may cause an allergic reaction in latex-sensitive individuals. The safe use of COSENTYX Sensoready pen or prefilled syringe in latex-sensitive individuals has not been studied.
5.6 Immunizations
Prior to initiating therapy with COSENTYX, consider completion of all age appropriate immunizations according to current immunization guidelines. COSENTYX may alter a patient`s immune response to live vaccines. Avoid use of live vaccines in patients treated with COSENTYX.
6 Adverse Reactions
The following adverse reactions are discussed in greater detail elsewhere in the labeling:
- Infections [see Warnings and Precautions (5.1)]
- Inflammatory Bowel Disease [see Warnings and Precautions (5.3)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Plaque Psoriasis
A total of 3430 plaque psoriasis subjects were treated with COSENTYX in controlled and uncontrolled clinical trials. Of these, 1641 subjects were exposed for at least 1 year.
Four placebo-controlled Phase 3 trials in plaque psoriasis subjects were pooled to evaluate the safety of COSENTYX in comparison to placebo up to 12 weeks after treatment initiation, in Trials PsO1, PsO2, PsO3, and PsO4. In total, 2077 subjects were evaluated (691 to COSENTYX 300 mg group, 692 to COSENTYX 150 mg group, and 694 to placebo group). Subjects randomized to COSENTYX received 300 mg or 150 mg doses subcutaneously at Weeks 0, 1, 2, 3, and 4 followed by the same dose every 4 weeks [see Clinical Studies (14)].
Table 2 summarizes the adverse reactions that occurred at a rate of at least 1% and at a higher rate in the COSENTYX groups than the placebo group during the 12-week placebo-controlled period of the placebo-controlled trials.
| COSENTYX | |||
| Adverse Reactions | 300 mg (N = 691) n (%) | 150 mg (N = 692) n (%) | Placebo (N = 694) n (%) |
| Nasopharyngitis | 79 (11.4) | 85 (12.3) | 60 (8.6) |
| Diarrhea | 28 (4.1) | 18 (2.6) | 10 (1.4) |
| Upper respiratory tract infection | 17 (2.5) | 22 (3.2) | 5 (0.7) |
| Rhinitis | 10 (1.4) | 10 (1.4) | 5 (0.7) |
| Oral herpes | 9 (1.3) | 1 (0.1) | 2 (0.3) |
| Pharyngitis | 8 (1.2) | 7 (1.0) | 0 (0) |
| Urticaria | 4 (0.6) | 8 (1.2) | 1 (0.1) |
| Rhinorrhea | 8 (1.2) | 2 (0.3) | 1 (0.1) |
Adverse reactions that occurred at rates less than 1% in the placebo-controlled period of Trials PsO1, PsO2, PsO3, and PsO4 through Week 12 included: sinusitis, tinea pedis, conjunctivitis, tonsillitis, oral candidiasis, impetigo, otitis media, otitis externa, inflammatory bowel disease, increased liver transaminases, and neutropenia.
Infections
In the placebo-controlled period of the clinical trials in plaque psoriasis (a total of 1382 subjects treated with COSENTYX and 694 subjects treated with placebo up to 12 weeks), infections were reported in 28.7% of subjects treated with COSENTYX compared with 18.9% of subjects treated with placebo. Serious infections occurred in 0.14% of subjects treated with COSENTYX and in 0.3% of subjects treated with placebo.
Over the entire treatment period (a total of 3430 plaque psoriasis subjects treated with COSENTYX for up to 52 weeks for the majority of subjects), infections were reported in 47.5% of subjects treated with COSENTYX (0.9 per patient-year of follow-up). Serious infections were reported in 1.2% of subjects treated with COSENTYX (0.015 per patient-year of follow-up).
Phase 3 data showed an increasing trend for some types of infection with increasing serum concentration of secukinumab. Candida infections, herpes viral infections, staphylococcal skin infections, and infections requiring treatment increased as serum concentration of secukinumab increased.
In the psoriasis open-label extension of Trials PsO1 and PsO2 (median follow-up of 3.9 years), representing 3582 subject-years of exposure, 74% of COSENTYX treated subjects reported infections (55 per 100 patient-years). Serious infections were reported in 4.5% of subjects (1.4 per 100 patient-years). Sepsis was reported in 5 subjects (0.2 per 100 patient-years).
Neutropenia was observed in controlled portion of clinical trials. Most cases of secukinumab-associated neutropenia were transient and reversible. No serious infections were associated with cases of neutropenia.
In the open-label extension of Trials PsO1 and PsO2, neutropenia (ANC < 1 x109/L) was reported in 1% of COSENTYX treated subjects (0.3 per 100 patient-years). Some cases of serious infections were associated with neutropenia; however the causal relationship was not established.
Inflammatory Bowel Disease
Cases of inflammatory bowel disease, in some cases serious, were observed in clinical trials with COSENTYX. In the plaque psoriasis program, with 3430 subjects exposed to COSENTYX over the entire treatment period for up to 52 weeks (2725 patient-years), there were 3 cases (0.11 per 100 patient-years) of exacerbation of Crohn’s disease, 2 cases (0.08 per 100 patient-years) of exacerbation of ulcerative colitis, and 2 cases (0.08 per 100 patient-years) of new onset ulcerative colitis. There were no cases in placebo subjects (N = 793; 176 patient-years) during the 12-week placebo-controlled period.
One case of exacerbation of Crohn’s disease was reported in open-labeled portions of clinical trials in plaque psoriasis.
Hypersensitivity Reactions
Anaphylaxis and cases of urticaria occurred in COSENTYX treated subjects in clinical trials [see Warnings and Precautions (5.4)].
Pediatric Plaque Psoriasis
The safety of COSENTYX was assessed in two Phase 3 trials in pediatric subjects with plaque psoriasis.
The first was a randomized, double-blind, placebo and active-controlled, 236-week trial (Trial PsO6) that enrolled 162 pediatric subjects 6 years of age and older, with severe plaque psoriasis (defined by PASI score ≥ 20, an IGA modified 2011 score of 4, and involving ≥ 10% of the body surface area) who were candidates for systemic therapy. The 162 subjects were randomized to receive placebo, a biologic active control, or COSENTYX. In the COSENTYX groups, subjects with body weight < 25 kg received 75 mg, subjects with body weight 25 to < 50 kg received either 75 mg or 150 mg (2 times the recommended dose), and subjects with body weight ≥ 50 kg received either 150 mg or 300 mg (2 times the recommended dose).
The second trial was a randomized, open-label, 208-week trial (Trial PsO7; NCT03668613) of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis (defined by a PASI score ≥ 12, IGA mod 2011 score of ≥ 3, and BSA involvement of ≥ 10% at randomization) who were randomized into two COSENTYX arms [Arm 1: 75 mg for body weight (BW) < 50 kg or 150 mg for ≥ 50 kg and Arm 2: 75 mg for BW < 25 kg, 150 mg for BW ≥ 25 kg and < 50 kg, or 300 mg for BW ≥ 50 kg].
The safety profile reported in these trials was consistent with the safety profile reported in adult plaque psoriasis trials.
Infections
One case of methicillin-resistant Staphylococcus aureus (MRSA) toxic shock syndrome (TSS) was reported in a COSENTYX treated subject during the placebo-controlled period.
In the pediatric safety pool, which includes all subjects who took at least one dose of COSENTYX during the treatment periods [198 subjects (287 patient years)], 22 (11%) subjects reported ≥ CTCAE Grade 2 neutropenia (≥1,000 to < 1,500 cells/mm3) with 57% of subjects followed for one year or more and 30% of subjects followed for two years or more. During the placebo-controlled period which included a total of 80 subjects treated with secukinumab and 41 subjects treated with placebo up to 12 weeks, ≥ CTCAE Grade 2 neutropenia was reported in 3 (4%) of the subjects treated with secukinumab compared with no subjects treated with placebo. No serious infections were associated with cases of neutropenia.
Psoriatic Arthritis
COSENTYX was studied in two placebo-controlled psoriatic arthritis trials with 1003 patients (703 patients on COSENTYX and 300 patients on placebo). Of the 703 patients who received COSENTYX, 299 patients received a subcutaneous loading dose of COSENTYX (PsA1) and 404 patients received an intravenous loading dose of secukinumab (PsA2) followed by COSENTYX administered by subcutaneous injection every four weeks. During the 16-week placebo-controlled period of the trials in patients with psoriatic arthritis, the overall proportion of patients with adverse events was similar in the secukinumab and placebo-treatment groups (59% and 58%, respectively). The adverse events that occurred at a proportion of at least 2% and at a higher proportion in the COSENTYX groups than the placebo groups during the 16-week placebo-controlled period were nasopharyngitis, upper respiratory tract infection, headache, nausea, and hypercholesterolemia. The safety profile observed in patients with psoriatic arthritis treated with COSENTYX is consistent with the safety profile in psoriasis.
Similar to the clinical trials in patients with psoriasis, there was an increased proportion of patients with infections in the COSENTYX groups (29%) compared to placebo group (26%).
There were cases of Crohn’s disease and ulcerative colitis that include patients who experienced either exacerbations or the development of new disease. There were three cases of inflammatory bowel disease, of which two patients received secukinumab and one received placebo.
Ankylosing Spondylitis
COSENTYX was studied in two placebo-controlled ankylosing spondylitis trials with 590 patients (394 patients on COSENTYX and 196 patients on placebo). Of the 394 patients who received COSENTYX, 145 patients received a subcutaneous load of COSENTYX (study AS1), and 249 received an intravenous loading dose of secukinumab (study AS2) followed by COSENTYX administered by subcutaneous injection every four weeks. During the 16-week placebo-controlled period of the trials in patients with ankylosing spondylitis, the overall proportion of patients with adverse events was higher in the secukinumab groups than the placebo-treatment groups (66% and 59%, respectively). The adverse events that occurred at a proportion of at least 2% and at a higher proportion in the COSENTYX groups than the placebo groups during the 16-week placebo-controlled period were nasopharyngitis, nausea, and upper respiratory tract infection. The safety profile observed in patients with ankylosing spondylitis treated with COSENTYX is consistent with the safety profile in psoriasis. In a third controlled study of AS (study AS3), the safety profile of the 300 mg dose of COSENTYX was consistent with the safety profile of the 150 mg dose of COSENTYX.
Similar to clinical trials in patients with psoriasis, there was an increased proportion of patients with infections in the COSENTYX groups (31%) compared to the placebo group (18%).
In the original ankylosing spondylitis program, with 571 patients exposed to COSENTYX there were 8 cases of inflammatory bowel disease during the entire treatment period [5 Crohn’s (0.7 per 100 patient-years) and 3 ulcerative colitis (0.4 per 100 patient-years)]. During the placebo-controlled 16-week period, there were 2 Crohn’s disease exacerbations and 1 new onset ulcerative colitis case that was a serious adverse event in patients treated with COSENTYX compared to none of the patients treated with placebo. During the remainder of the study when all patients received COSENTYX, 1 patient developed Crohn’s disease, 2 patients had Crohn’s exacerbations, 1 patient developed ulcerative colitis, and 1 patient had an ulcerative colitis exacerbation.
Non-Radiographic Axial Spondyloarthritis
COSENTYX was studied in one randomized, double-blind, placebo-controlled non-radiographic axial spondyloarthritis trial with 555 patients (185 patients on with load COSENTYX, 184 patients on without load COSENTYX and 186 patients on placebo). The safety profile for patients with nr-axSpA treated with COSENTYX was overall similar to the safety profile seen in patients with AS and other previous experience with COSENTYX. Patients in nr-axSpA1 study who received the loading dosing regimen compared to those without the loading regimen, had higher incidence of infections and infestations (92 per 100 patient-years vs 72 per 100 patient years), including nasopharyngitis, upper respiratory tract infection and urinary tract infection, and gastrointestinal disorders (27 per 100 patient-years vs 22 per 100 patient-years), including gastritis, lower abdominal pain, colitis, diarrhea, and hematochezia.
6.2 Immunogenicity
As with all therapeutic proteins, there is the potential for immunogenicity. The immunogenicity of COSENTYX was evaluated using an electrochemiluminescence-based bridging immunoassay. Less than 1% of subjects treated with COSENTYX developed antibodies to secukinumab in up to 52 weeks of treatment. However, this assay has limitations in detecting anti-secukinumab antibodies in the presence of secukinumab; therefore, the incidence of antibody development might not have been reliably determined. Of the subjects who developed antidrug antibodies, approximately one-half had antibodies that were classified as neutralizing. Neutralizing antibodies were not associated with loss of efficacy.
The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to COSENTYX with the incidences of antibodies to other products may be misleading.
7 Drug Interactions
CYP450 Substrates
The formation of CYP450 enzymes can be altered by increased levels of certain cytokines (e.g., IL-1, IL-6, IL-10, TNFα, IFN) during chronic inflammation.
Upon initiation or discontinuation of COSENTYX in patients who are receiving concomitant CYP450 substrates, particularly those with a narrow therapeutic index, consider monitoring for therapeutic effect or drug concentration and consider dosage adjustment of the CYP450 substrate as needed [see Clinical Pharmacology (12.3)].
8.1 Pregnancy
Risk Summary
Limited available human data with COSENTYX use in pregnant women are insufficient to inform a drug-associated risk of adverse developmental outcomes. In an embryo-fetal development study, no adverse developmental effects were observed in infants born to pregnant monkeys after subcutaneous administration of secukinumab during organogenesis at doses up to 30 times the maximum recommended human dose (MRHD) (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown; however, the background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data
Animal Data
An embryo-fetal development study was performed in cynomolgus monkeys with secukinumab. No malformations or embryo-fetal toxicity were observed in fetuses from pregnant monkeys that were administered secukinumab weekly by the subcutaneous route during the period of organogenesis at doses up to 30 times the MRHD (on a mg/kg basis at a maternal dose of 150 mg/kg).
A pre- and post-natal development toxicity study was performed in mice with a murine analog of secukinumab. No treatment-related effects on functional, morphological or immunological development were observed in fetuses from pregnant mice that were administered the murine analog of secukinumab on gestation days 6, 11, and 17 and on postpartum days 4, 10, and 16 at doses up to 150 mg/kg/dose.
8.2 Lactation
Risk Summary
It is not known whether secukinumab is excreted in human milk or absorbed systemically after ingestion. There are no data on the effects of COSENTYX on the breastfed child or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for COSENTYX and any potential adverse effects on the breastfed child from COSENTYX or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of COSENTYX have been established in pediatric subjects aged 6 years and older with moderate to severe plaque psoriasis [see Adverse Reactions (6.1), Clinical Studies (14.2)]. Safety and effectiveness of COSENYX in pediatric patients with plaque psoriasis below the age of 6 years have not been established.
The safety and effectiveness of COSENTYX in pediatric patients in other indications have not been established.
8.5 Geriatric Use
Of the 3430 plaque psoriasis subjects exposed to COSENTYX in clinical trials, a total of 230 were 65 years or older, and 32 subjects were 75 years or older. Although no differences in safety or efficacy were observed between older and younger subjects, the number of subjects aged 65 years and older was not sufficient to determine whether they responded differently from younger subjects.
10 Overdosage
Doses up to 30 mg/kg intravenously have been administered in clinical trials without dose-limiting toxicity. In the event of overdosage, it is recommended that the patient be monitored for any signs or symptoms of adverse reactions and appropriate symptomatic treatment be instituted immediately.
11 Description
Secukinumab, a recombinant human monoclonal IgG1/κ antibody, is an interleukin-17A antagonist. It is expressed in a recombinant Chinese Hamster Ovary (CHO) cell line. Secukinumab has a molecular mass of approximately 151 kDa; both heavy chains of secukinumab contain oligosaccharide chains.
COSENTYX Injection
COSENTYX injection is a sterile, preservative-free, clear to slightly opalescent, colorless to slightly yellow solution for subcutaneous use. COSENTYX is supplied in a single-dose Sensoready pen with a 27-gauge fixed ½-inch needle, or a single-dose prefilled syringe with a 27-gauge fixed ½-inch needle. The removable cap of the COSENTYX Sensoready pen or prefilled syringe contains natural rubber latex.
Each COSENTYX Sensoready pen or prefilled syringe contains 150 mg of secukinumab formulated in: L-histidine/histidine hydrochloride monohydrate (3.103 mg), L-methionine (0.746 mg), polysorbate 80 (0.2 mg), trehalose dihydrate (75.67 mg), and Sterile Water for Injection, USP, at pH of 5.8.
Each COSENTYX 75 mg/0.5 mL prefilled syringe contains 75 mg of secukinumab formulated in: L-histidine/histidine hydrochloride monohydrate (1.552 mg), L-methionine (0.373 mg), polysorbate 80 (0.1 mg), trehalose dihydrate (37.83 mg), and Sterile Water for Injection, USP, at pH of 5.8.
COSENTYX for Injection
COSENTYX for injection is supplied as a sterile, preservative free, white to slightly yellow, lyophilized powder in single-dose vials for subcutaneous use after reconstitution. Each COSENTYX vial contains 150 mg of secukinumab formulated in L-histidine/histidine hydrochloride monohydrate (4.656 mg), polysorbate 80 (0.6 mg), and sucrose (92.43 mg). Following reconstitution with 1 mL Sterile Water for Injection, USP, the resulting pH is approximately 5.8.
12.1 Mechanism Of Action
Secukinumab is a human IgG1 monoclonal antibody that selectively binds to the interleukin-17A (IL-17A) cytokine and inhibits its interaction with the IL-17 receptor. IL-17A is a naturally occurring cytokine that is involved in normal inflammatory and immune responses. Secukinumab inhibits the release of proinflammatory cytokines and chemokines.
12.2 Pharmacodynamics
Elevated levels of IL-17A are found in psoriatic plaques. Treatment with COSENTYX may reduce epidermal neutrophils and IL-17A levels in psoriatic plaques. Serum levels of total IL-17A (free and secukinumab-bound IL-17A) measured at Week 4 and Week 12 were increased following secukinumab treatment. These pharmacodynamic activities are based on small exploratory studies. The relationship between these pharmacodynamic activities and the mechanism(s) by which secukinumab exerts its clinical effects is unknown.
Increased numbers of IL-17A producing lymphocytes and innate immune cells and increased levels of IL-17A have been found in the blood of patients with psoriatic arthritis and ankylosing spondylitis. Increased numbers of IL-17A producing lymphocytes have also been found in patients with non-radiographic axial spondyloarthritis.
Immune Response to Non-Live Vaccines During Treatment
Healthy individuals who received a single 150 mg dose of COSENTYX 2 weeks prior to vaccination with a non-U.S. approved group C meningococcal polysaccharide conjugate vaccine and a non-U.S. approved inactivated seasonal influenza vaccine had similar antibody responses compared to individuals who did not receive COSENTYX prior to vaccination. The clinical effectiveness of meningococcal and influenza vaccines has not been assessed in patients undergoing treatment with COSENTYX [see Warnings and Precautions (5.6)].
12.3 Pharmacokinetics
The pharmacokinetic (PK) properties of secukinumab observed in psoriatic arthritis, ankylosing spondylitis and non-radiographic axial spondyloarthritis patients were similar to the PK properties displayed in plaque psoriasis patients.
Absorption
Following a single subcutaneous dose of either 150 mg (one-half the recommended dose) or 300 mg in plaque psoriasis subjects, secukinumab reached peak mean (± SD) serum concentrations (Cmax) of 13.7 ± 4.8 mcg/mL and 27.3 ± 9.5 mcg/mL, respectively, by approximately 6 days post dose.
Following multiple subcutaneous doses of secukinumab, the mean (± SD) serum trough concentrations of secukinumab ranged from 22.8 ± 10.2 mcg/mL (150 mg) to 45.4 ± 21.2 mcg/mL (300 mg) at Week 12. At the 300 mg dose at Week 4 and Week 12, the mean trough concentrations resulted from the Sensoready pen were 23% to 30% higher than those from the lyophilized powder and 23% to 26% higher than those from the prefilled syringe based on cross-study comparisons.
Steady-state concentrations of secukinumab were achieved by Week 24 following the every 4-week dosing regimens. The mean (± SD) steady-state trough concentrations ranged from 16.7 ± 8.2 mcg/mL (150 mg) to 34.4 ± 16.6 mcg/mL (300 mg).
In healthy subjects and subjects with plaque psoriasis, secukinumab bioavailability ranged from 55% to 77% following subcutaneous dose of 150 mg (one-half the recommended dose) or 300 mg.
Distribution
The mean volume of distribution during the terminal phase (Vz) following a single intravenous administration ranged from 7.10 to 8.60 L in plaque psoriasis subjects. Intravenous use is not recommended [see Dosage and Administration (2)].
Secukinumab concentrations in interstitial fluid in lesional and non-lesional skin of plaque psoriasis subjects ranged from 27% to 40% of those in serum at 1 and 2 weeks after a single subcutaneous dose of secukinumab 300 mg.
Elimination
Metabolism
The metabolic pathway of secukinumab has not been characterized. As a human IgG1κ monoclonal antibody secukinumab is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
Excretion
The mean systemic clearance (CL) ranged from 0.14 L/day to 0.22 L/day and the mean half-life ranged from 22 to 31 days in plaque psoriasis subjects following intravenous and subcutaneous administration across all psoriasis trials. Intravenous use is not recommended [see Dosage and Administration (2)].
Dose Linearity
Secukinumab exhibited dose-proportional pharmacokinetics in subjects with psoriasis over a dose range from 25 mg (approximately 0.083 times the recommended dose) to 300 mg following subcutaneous administrations.
Weight
Secukinumab clearance and volume of distribution increase as body weight increases.
Specific Populations
Patients with Hepatic or Renal Impairment
No formal trial of the effect of hepatic or renal impairment on the pharmacokinetics of secukinumab was conducted.
Geriatric Patients
Population pharmacokinetic analysis indicated that the clearance of secukinumab was not significantly influenced by age in adult subjects with plaque psoriasis, psoriatic arthritis and ankylosing spondylitis. Subjects who are 65 years or older had apparent clearance of secukinumab similar to subjects less than 65 years old.
Pediatric Patients
In a pool of the two pediatric trials, subjects with moderate to severe plaque psoriasis (6 years of age and older) were administered secukinumab at the recommended pediatric dosing regimen. At Week 24, secukinumab steady state mean ± SD serum trough concentrations were 32.6 ± 10.8 mcg/mL (n = 8), 19.8 ± 6.96 mcg/mL (n = 24), and 27.3 ± 10.1 mcg/mL (n = 36), in subjects weighing < 25 kg and receiving 75 mg of secukinumab, subjects weighing ≥ 25 and < 50 kg and receiving 75 mg of secukinumab, and subjects weighing ≥ 50 kg and receiving 150 mg of secukinumab, respectively.
Drug Interactions
Cytochrome P450 Substrates
In adult subjects with plaque psoriasis, midazolam (CYP3A4 substrate) pharmacokinetics was similar when administered alone, or when administered following either a single or five weekly subcutaneous administrations of 300 mg secukinumab [see Drug Interactions (7.3)].
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Animal studies have not been conducted to evaluate the carcinogenic or mutagenic potential of COSENTYX. Some published literature suggests that IL-17A directly promotes cancer cell invasion in vitro, whereas other reports indicate IL-17A promotes T-cell mediated tumor rejection. Depletion of IL-17A with a neutralizing antibody inhibited tumor development in mice. The relevance of experimental findings in mouse models for malignancy risk in humans is unknown.
No effects on fertility were observed in male and female mice that were administered a murine analog of secukinumab at subcutaneous doses up to 150 mg/kg once weekly prior to and during the mating period.
14.1 Adult Plaque Psoriasis
Four multicenter, randomized, double-blind, placebo-controlled trials (Trials PsO1, PsO2, PsO3, and PsO4) enrolled 2403 subjects (691 randomized to COSENTYX 300 mg, 692 to COSENTYX 150 mg, 694 to placebo, and 323 to a biologic active control) 18 years of age and older with plaque psoriasis who had a minimum body surface area involvement of 10%, and Psoriasis Area and Severity Index (PASI) score greater than or equal to 12, and who were candidates for phototherapy or systemic therapy.
- Trial PsO1 (NCT01365455) enrolled 738 subjects (245 randomized to COSENTYX 300 mg, 245 to COSENTYX 150 mg, and 248 to placebo). Subjects received subcutaneous treatment at Weeks 0, 1, 2, 3, and 4 followed by dosing every 4 weeks. Subjects randomized to COSENTYX received 300 mg or 150 mg doses at Weeks 0, 1, 2, 3, and 4 followed by the same dose every 4 weeks. Subjects randomized to receive placebo that were non-responders at Week 12 were then crossed over to receive COSENTYX (either 300 mg or 150 mg) at Weeks 12, 13, 14, 15, and 16 followed by the same dose every 4 weeks. All subjects were followed for up to 52 weeks following first administration of study treatment.
- Trial PsO2 (NCT01358578) enrolled 1306 subjects (327 randomized to COSENTYX 300 mg, 327 to COSENTYX 150 mg, 326 to placebo, and 323 to a biologic active control). COSENTYX and placebo data are described. Subjects received subcutaneous treatment at Weeks 0, 1, 2, 3, and 4 followed by dosing every 4 weeks. Subjects randomized to COSENTYX received 300 mg or 150 mg doses at Weeks 0, 1, 2, 3, and 4 followed by the same dose every 4 weeks. Subjects randomized to receive placebo that were non-responders at Week 12 then crossed over to receive COSENTYX (either 300 mg or 150 mg) at Weeks 12, 13, 14, 15, and 16 followed by the same dose every 4 weeks. All subjects were followed for up to 52 weeks following first administration of study treatment.
- Trial PsO3 (NCT01555125) enrolled 177 subjects (59 randomized to COSENTYX 300 mg, 59 to COSENTYX 150 mg, and 59 to placebo) and assessed safety, tolerability, and usability of COSENTYX self-administration via prefilled syringe for 12 weeks. Subjects received subcutaneous treatment at Weeks 0, 1, 2, 3, and 4, followed by the same dose every 4 weeks for up to 12 weeks total.
- Trial PsO4 (NCT01636687) enrolled 182 subjects (60 randomized to COSENTYX 300 mg, 61 to COSENTYX 150 mg, and 61 to placebo) and assessed safety, tolerability, and usability of COSENTYX self-administration via Sensoready pen for 12 weeks. Subjects received subcutaneous treatment at Weeks 0, 1, 2, 3, and 4, followed by the same dose every 4 weeks for up to 12 weeks total.
Endpoints
In all trials, the endpoints were the proportion of subjects who achieved a reduction in PASI score of at least 75% (PASI 75) from baseline to Week 12 and treatment success (clear or almost clear) on the Investigator’s Global Assessment modified 2011 (IGA). Other evaluated outcomes included the proportion of subjects who achieved a reduction in PASI score of at least 90% (PASI 90) from baseline at Week 12, maintenance of efficacy to Week 52, and improvements in itching, pain, and scaling at Week 12 based on the Psoriasis Symptom Diary©.
The PASI is a composite score that takes into consideration both the percentage of body surface area affected and the nature and severity of psoriatic changes within the affected regions (induration, erythema and scaling). The IGA is a 5-category scale, including “0 = clear”, “1 = almost clear”, “2 = mild”, “3 = moderate” or “4 = severe” indicating the physician’s overall assessment of the psoriasis severity focusing on induration, erythema and scaling. Treatment success of “clear” or “almost clear” consisted of no signs of psoriasis or normal to pink coloration of lesions, no thickening of the plaque, and none to minimal focal scaling.
Baseline Characteristics
Across all treatment groups the baseline PASI score ranged from 11 to 72 with a median of 20 and the baseline IGA score ranged from “moderate” (62%) to “severe” (38%). Of the 2077 plaque psoriasis subjects who were included in the placebo-controlled trials, 79% were biologic-naïve (have never received a prior treatment with biologics) and 45% were non-biologic failures (failed to respond to a prior treatment with non-biologic therapies). Of the subjects who received a prior treatment with biologics, over one-third were biologic failures. Approximately 15% to 25% of trial subjects had a history of psoriatic arthritis.
Clinical Response
The results of Trials PsO1 and PsO2 are presented in Table 3.
| Trial PsO1 | Trial PsO2 | |||||
| COSENTYX 300 mg (N = 245) n (%) | COSENTYX 150 mg (N = 245) n (%) | Placebo (N = 248) n (%) | COSENTYX 300 mg (N = 327) n (%) | COSENTYX 150 mg (N = 327) n (%) | Placebo (N = 326) n (%) | |
| PASI 75 response | 200 (82) | 174 (71) | 11 (4) | 249 (76) | 219 (67) | 16 (5) |
| IGA of clear or almost clear | 160 (65) | 125 (51) | 6 (2) | 202 (62) | 167 (51) | 9 (3) |
The results of Trials PsO3 and PsO4 are presented in Table 4.
| Trial PsO3 | Trial PsO4 | |||||
| COSENTYX 300 mg (N = 59) n (%) | COSENTYX 150 mg (N = 59) n (%) | Placebo (N = 59) n (%) | COSENTYX 300 mg (N = 60) n (%) | COSENTYX 150 mg (N = 61) n (%) | Placebo (N = 61) n (%) | |
| PASI 75 response | 44 (75) | 41 (69) | 0 (0) | 52 (87) | 43 (70) | 2 (3) |
| IGA of clear or almost clear | 40 (68) | 31 (53) | 0 (0) | 44 (73) | 32 (52) | 0 (0) |
Examination of age, gender, and race subgroups did not identify differences in response to COSENTYX among these subgroups. Based on post-hoc sub-group analyses in subjects with moderate to severe psoriasis, subjects with lower body weight and lower disease severity may achieve an acceptable response with COSENTYX 150 mg.
PASI 90 response at Week 12 was achieved with COSENTYX 300 mg and 150 mg compared to placebo in 59% (145/245) and 39% (95/245) versus 1% (3/248) of subjects, respectively (Trial PsO1) and 54% (175/327) and 42% (137/327) versus 2% (5/326) of subjects, respectively (Trial PsO2). Similar results were seen in Trials PsO3 and PsO4.
With continued treatment over 52 weeks, subjects in Trial PsO1 who were PASI 75 responders at Week 12 maintained their responses in 81% (161/200) of the subjects treated with COSENTYX 300 mg and in 72% (126/174) of subjects treated with COSENTYX 150 mg. Trial PsO1 subjects who were clear or almost clear on the IGA at Week 12 also maintained their responses in 74% (119/160) of subjects treated with COSENTYX 300 mg and in 59% (74/125) of subjects treated with COSENTYX 150 mg. Similarly in Trial PsO2, PASI 75 responders maintained their responses in 84% (210/249) of subjects treated with COSENTYX 300 mg and in 82% (180/219) of subjects treated with COSENTYX 150 mg. Trial PsO2 subjects who were clear or almost clear on the IGA also maintained their responses in 80% (161/202) of subjects treated with COSENTYX 300 mg and in 68% (113/167) of subjects treated with COSENTYX 150 mg.
Among the subjects who chose to participate (39%) in assessments of patient reported outcomes, improvements in signs and symptoms related to itching, pain, and scaling, at Week 12 compared to placebo (Trials PsO1 and PsO2) were observed using the Psoriasis Symptom Diary©.
Psoriasis Lesions of Scalp
A randomized, placebo-controlled trial (Trial PsO5; NCT02267135) enrolled 102 subjects with moderate to severe psoriasis lesions of scalp, defined as having a Psoriasis Scalp Severity Index (PSSI) score of greater than or equal to 12, an IGA scalp only score of 3 or greater, and at least 30% of the scalp affected. In this trial, 62% of subjects had at least 50% of scalp surface area affected. The proportions of subjects achieving an IGA scalp only score of 0 or 1 (clear or almost clear) were 56.9% and 5.9% for the COSENTYX 300 mg and the placebo groups, respectively.
14.2 Pediatric Plaque Psoriasis
A 52-week, multicenter randomized, double-blind, placebo and active-controlled trial (Trial PsO6; NCT02471144) enrolled 162 pediatric subjects 6 years of age and older, with severe plaque psoriasis (as defined by a PASI score ≥ 20, an IGA modified 2011 score of 4, and involving ≥ 10% of the body surface area) who were candidates for systemic therapy.
Subjects were randomized to receive placebo, COSENTYX, or a biologic active control. In the COSENTYX groups, subjects with body weight < 25 kg received 75 mg, subjects with body weight 25 to < 50 kg received either 75 mg or 150 mg (2 times the recommended dose), and subjects with body weight ≥ 50 kg received either 150 mg or 300 mg (2 times the recommended dose). Subjects in the COSENTYX and placebo groups received treatment at Weeks 0, 1, 2, 3, and 4 followed by dosing every 4 weeks. At Week 12, subjects randomized to placebo who were non-responders were switched to COSENTYX (dose based on body weight) and received COSENTYX at Weeks 12, 13, 14, and 15, followed by the same dose every 4 weeks starting at Week 16.
Overall, 60% of the subjects were female, 83% were Caucasian, the median body weight was 50.6 kg, and the mean age was 13.5 years with 23% of the subjects < 12 years. At baseline, the median PASI score was 26 (ranged from 17 to 60), and 99% of the subjects had an IGA modified 2011 score of 4 (‘severe’). Approximately 43% of the subjects had prior exposure to phototherapy, 53% to conventional systemic therapy, 3% to biologics, and 9% had concomitant psoriatic arthritis.
The co-primary endpoints were the proportion of subjects who achieved a reduction in PASI score of at least 75% (PASI 75) from baseline to Week 12 and the proportion of subjects who achieved an IGA modified 2011 score of ‘clear’ or ‘almost clear’ (0 or 1) with at least a 2 point improvement from baseline to Week 12. The key secondary endpoint was the proportion of subjects who achieved a reduction in PASI score of at least 90% (PASI 90) from baseline to Week 12.
Clinical Response
Table 5 presents the efficacy results at Week 12 by baseline weight strata for the approved dose.
| Non-responder imputation was used to handle missing values. aCOSENTYX treated subjects received 75 mg for subjects < 50 kg and 150 mg for subjects ≥ 50 kg body weight. | ||||||
| Body Weight < 50 kg | Body Weight ≥ 50 kg | Total | ||||
| COSENTYX 75 mg (N = 22) n (%) | Placebo (N = 20) n (%) | COSENTYX 150 mg (N = 21) n (%) | Placebo (N = 21) n (%) | COSENTYXa (N = 43) n (%) | Placebo (N = 41) n (%) | |
| IGA of clear or almost clear | 7 (32) | 1 (5) | 17 (81) | 1 (5) | 24 (56) | 2 (5) |
| PASI 75 response | 12 (55) | 2 (10) | 18 (86) | 4 (19) | 30 (70) | 6 (15) |
| PASI 90 response | 9 (41) | 1 (5) | 17 (81) | 0 (0) | 26 (60) | 1 (2) |
14.3 Psoriatic Arthritis
The safety and efficacy of COSENTYX were assessed in 1999 patients, in 3 randomized, double-blind, placebo-controlled studies (PsA1, PsA2 and PsA3) in adult patients, age 18 years and older with active psoriatic arthritis (greater than or equal to 3 swollen and greater than or equal to 3 tender joints) despite non-steroidal anti-inflammatory drug (NSAID), corticosteroid or disease modifying anti-rheumatic drug (DMARD) therapy. Patients in these studies had a diagnosis of PsA of at least 5 years across all studies. At baseline, over 61% and 42% of the patients had enthesitis and dactylitis, respectively. Overall, 31% of patients discontinued previous treatment with anti-TNFα agents due to either lack of efficacy or intolerance. In addition, approximately 53% of patients from both studies had concomitant methotrexate (MTX) use. Patients with different subtypes of PsA were enrolled, including polyarticular arthritis with no evidence of rheumatoid nodules (80%), asymmetric peripheral arthritis (63%), distal interphalangeal involvement (58%), spondylitis with peripheral arthritis (20%) and arthritis mutilans (7%).
PsA1 Study (NCT 01752634) evaluated 397 patients, who were treated with COSENTYX 75 mg, 150 mg or 300 mg subcutaneous treatment at Weeks 0, 1, 2, 3 and 4, followed by the same dose every 4 weeks. Patients receiving placebo were re-randomized to receive COSENTYX (either 150 mg or 300 mg every 4 weeks) at Week 16 or Week 24 based on responder status. The primary endpoint was the percentage of patients achieving an ACR20 response at Week 24.
PsA2 Study (NCT 01392326) evaluated 606 patients, who were treated with secukinumab 10 mg/kg, intravenous treatment (or placebo) at Weeks 0, 2, and 4, followed by either 75 mg or 150 mg subcutaneous COSENTYX treatment (or placebo) every 4 weeks. Patients receiving placebo were re-randomized to receive COSENTYX (either 75 mg or 150 mg every 4 weeks) at Week 16 or Week 24 based on responder status.
PsA3 Study (NCT 02404350) evaluated 996 patients, who were treated with COSENTYX 150 mg or 300 mg subcutaneous treatment at Weeks 0, 1, 2, 3, and 4 followed by the same dose every 4 weeks, or once every 4 weeks of COSENTYX 150 mg. Patients treated with placebo received COSENTYX, either 150 mg or 300 mg, subcutaneous, per baseline randomization, at Week 16 or Week 24 based upon responder status. The primary endpoint was ACR20 response at Week 16 with the key secondary endpoint the change from baseline in modified Total Sharp Score (mTSS) at Week 24.
Clinical Response
In PsA1, patients treated with 150 mg or 300 mg COSENTYX demonstrated a greater clinical response, including ACR20, ACR50, and ACR70 compared to placebo at Week 24 (Table 6). Responses were similar in patients regardless of concomitant methotrexate treatment. Responses were seen regardless of prior anti-TNFα exposure.
In patients with coexistent plaque psoriasis receiving COSENTYX (n = 99), the skin lesions of psoriasis improved with treatment, relative to placebo, as measured by the Psoriasis Area Severity Index (PASI).
| aPatients who met escape criteria (less than 20% improvement in tender or swollen joint counts) at Week 16 were considered non-responders. | |||||
| COSENTYX | COSENTYX | Placebo | Difference from Placebo (95% CI) | ||
| 150 mg (N = 100) | 300 mg (N = 100) | (N = 98) | COSENTYX 150 mg | COSENTYX 300 mg | |
| ACR20 response | |||||
| Week 16 (%) | 60 | 57 | 18 | 42 (30, 54) | 38 (26, 51) |
| Week 24 (%) | 51 | 54 | 15 | 36 (24, 48) | 39 (27, 51) |
| ACR50 response | |||||
| Week 16 (%) | 37 | 35 | 6 | 31 (21, 42) | 28 (18, 39) |
| Week 24 (%) | 35 | 35 | 7 | 28 (18, 38) | 28 (17, 38) |
| ACR70 response | |||||
| Week 16 (%) | 17 | 15 | 2 | 15 (7, 23) | 13 (5, 20) |
| Week 24 (%) | 21 | 20 | 1 | 20 (12, 28) | 19 (11, 27) |
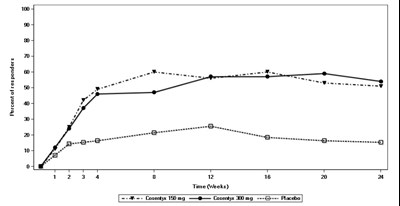
The percentage of patients achieving ACR20 response by visit is shown in Figure 1. Patients on placebo who received COSENTYX without a loading regimen achieved similar ACR20 responses over time (data not shown).
Figure 1: Percent of Patients Achieving ACR 20 Responsea in PsA1 Study Through Week 24
aPatients who met escape criteria (less than 20% improvement in tender or swollen joint counts) at Week 16 were considered non-responders.
The improvements in the components of the ACR response criteria are shown in Table 7.
| aWeek 16 rather than Week 24 data are displayed to provide comparison between arms prior to placebo escape to COSENTYX.
bMean Change based upon observed data. | |||
| COSENTYX 150 mg (N = 100) | COSENTYX 300 mg (N = 100) | Placebo (N = 98) | |
| No. of Swollen Joints | |||
| Baseline | 12.0 | 11.2 | 12.1 |
| Mean change at Week 16 | -4.86 | -5.83 | -3.22 |
| Number of Tender Joints | |||
| Baseline | 24.1 | 20.2 | 23.5 |
| Mean change at Week 16 | -10.70 | -10.01 | -1.77 |
| Patient’s Assessment of Pain | |||
| Baseline | 58.9 | 57.7 | 55.4 |
| Mean change at Week 16 | -22.91 | -23.97 | -7.98 |
| Patient Global Assessment | |||
| Baseline | 62.0 | 60.7 | 57.6 |
| Mean change at Week 16 | -25.47 | -25.40 | -8.25 |
| Physician Global Assessment | |||
| Baseline | 56.7 | 55.0 | 55.0 |
| Mean change at Week 16 | -29.24 | -34.71 | -14.95 |
| Disability Index (HAQ) | |||
| Baseline | 1.2200 | 1.2828 | 1.1684 |
| Mean change at Week 16 | -0.45 | -0.55 | -0.23 |
| CRP (mg/L) | |||
| Baseline | 14.15 | 10.88 | 7.87 |
| Mean Change at Week 16b | -8.41 | -7.21 | 0.79 |
Improvements in enthesitis and dactylitis scores were observed in each COSENTYX group compared to placebo at Week 24.
Radiographic Response
In PsA3 Study, inhibition of progression of structural damage was assessed radiographically and expressed by the modified mTSS and its components, the Erosion Score (ES) and Joint Space Narrowing Score (JSN), at Week 24 compared to baseline. Radiographs of hands, wrists, and feet were obtained at baseline, Week 16 and/or Week 24 and scored independently by at least two readers who were blinded to treatment group and visit number. COSENTYX 150 mg without load, 150 mg with load and 300 mg with load treatment significantly inhibited progression of peripheral joint damage compared with placebo treatment as measured by change from baseline in mTSS at Week 24. The percentage of patients with no disease progression (defined as a change from baseline in mTSS of less than or equal to 0.0) from randomization to Week 24 was 75.7%, 70.9%, and 76.5% for COSENTYX 150 mg without load, 150 mg, 300 mg, respectively versus 68.2% for placebo.
| Results from a linear mixed effects model that excluded data after escape for placebo subjects who received escape therapy at Week 16. The model assumes approximately linear progression over time and estimates a difference in rates (slopes) of progression over 24 weeks to compare treatment arms. | |||
| Treatment | N | Rate of Change per 24 weeks | Difference from Placebo (95% CI) |
| COSENTYX 150 mg without load | 210 | -0.10 | -0.61 (-0.95, -0.26) |
| COSENTYX 150 mg with load | 213 | 0.14 | -0.37 (-0.71, -0.03) |
| COSENTYX 300 mg with load | 217 | 0.03 | -0.48 (-0.82, -0.14) |
| Placebo | 296 | 0.51 | -- |
Physical Function
Improvement in physical function as assessed by Health Assessment Questionnaire-Disability Index (HAQ-DI) demonstrated that the proportion of patients who achieved at least -0.3 improvement in HAQ-DI score from baseline was greater in the COSENTYX 150 mg and 300 mg groups compared to placebo at Week 16 and 24. At Week 16 in PsA1 study, estimated mean change from baseline was -0.23 in the placebo group compared with -0.45 in the COSENTYX 150 mg group and -0.55 in the COSENTYX 300 mg group.
14.4 Ankylosing Spondylitis
The safety and efficacy of COSENTYX were assessed in 816 patients in three randomized, double-blind, placebo-controlled studies (AS1, AS2 and AS3) in adult patients 18 years of age and older with active ankylosing spondylitis. Patients had active disease as defined by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) greater or equal to 4 despite non-steroidal anti-inflammatory drug (NSAID), corticosteroid or disease modifying anti-rheumatic drug (DMARD) therapy. At baseline, approximately 13% and 25% used concomitant methotrexate or sulfasalazine, respectively. Overall, 29% of patients discontinued previous treatment with anti-TNFα agents due to either lack of efficacy or intolerance.
AS1 Study (NCT01649375) evaluated 219 patients, who were treated with COSENTYX 75 mg or 150 mg subcutaneous treatment at Weeks 0, 1, 2, 3, and 4, followed by the same dose every 4 weeks. At Week 16, patients receiving placebo were re-randomized to either COSENTYX 75 mg or 150 mg every 4 weeks. The primary endpoint was the percentage of patients achieving an ASAS20 response at Week 16.
AS2 Study (NCT01358175) evaluated 371 patients, who were treated with secukinumab 10 mg/kg intravenous treatment at Weeks 0, 2, and 4 (for both treatment arms) or placebo, followed by either 75 mg or 150 mg subcutaneous COSENTYX treatment every 4 weeks or placebo. Patients receiving placebo were re-randomized to receive COSENTYX (either 75 mg or 150 mg every 4 weeks) at Week 16 or Week 24 based on responder status.
AS3 Study (NCT02008916) evaluated 226 patients, who were treated with secukinumab 10 mg/kg intravenous treatment at Weeks 0, 2, and 4 (for both treatment arms) or placebo, followed by either 150 mg or 300 mg subcutaneous COSENTYX treatment every 4 weeks or placebo. Patients receiving placebo were re-randomized to receive COSENTYX (either 150 mg or 300 mg every 4 weeks) at Week 16. The primary endpoint was the percentage of patients achieving an ASAS20 response at Week 16. Patients were blinded to the treatment regimen up to Week 52, and the study continued to Week 156.
Clinical Response
In AS1, patients treated with 150 mg COSENTYX demonstrated greater improvements in ASAS20 and ASAS40 responses compared to placebo at Week 16 (Table 9). Responses were similar in patients regardless of concomitant therapies.
| COSENTYX 150 mg (n = 72) | Placebo (n = 74) | Difference from placebo (95% CI) | |
| ASAS20 response, % | 61 | 28 | 33 (18, 48) |
| ASAS40 response, % | 36 | 11 | 25 (12, 38) |
The improvements in the main components of the ASAS20 response criteria and other measures of disease activity are shown in Table 10.
| ||||
| COSENTYX 150 mg (N = 72) | Placebo (N = 74) | |||
| Baseline | Week 16 change from baseline | Baseline | Week 16 change from baseline | |
| ASAS20 Response criteria | ||||
| -Patient Global Assessment of Disease Activity (0-100 mm)1 | 67.5 | -27.7 | 70.5 | -12.9 |
| -Total spinal pain (0-100 mm) | 66.2 | -28.5 | 69.2 | -10.9 |
| -BASFI (0-10)2 | 6.2 | -2.2 | 6.1 | -0.7 |
| -Inflammation (0-10)3 | 6.5 | -2.5 | 6.5 | -0.8 |
| BASDAI Score4 | 6.6 | -2.2 | 6.8 | -0.9 |
| BASMI5 | 3.6 | -0.51 | 3.9 | -0.22 |
| hsCRP6 (mg/L) Mean Change at Week 16 | 27.0 | -17.2 | 15.9 | 0.8 |
The percent of patients achieving ASAS20 responses by visit is shown in Figure 2. Patients on placebo who received COSENTYX without a loading regimen achieved similar ASAS20 responses over time (data not shown).
Figure 2: ASAS20 Responses in all AS1 Study Patients Over Time Up to Week 16
In AS3 Study, patients treated with COSENTYX (150 mg and 300 mg) demonstrated improved signs and symptoms, and had comparable efficacy responses, regardless of dose, that were superior to placebo at Week 16 for the primary and most secondary endpoints. At Week 16, the ASAS20 and ASAS40 responses were 58.1% and 40.5% for 150 mg and 60.5% and 42.1% for 300 mg, respectively. The percent of patients achieving ASAS20 responses by visit is shown in Figure 3.
Figure 3: ASAS20 Responses in all AS3 Study Patients Over Time Up to Week 16
COSENTYX treated patients showed improvement compared to placebo-treated patients in health-related quality of life as assessed by ASQoL at Week 16.
14.5 Non-Radiographic Axial Spondyloarthritis
The safety and efficacy of COSENTYX were assessed in 555 patients in one randomized, double-blind, placebo-controlled Phase 3 study (nr-axSpA1, NCT02696031) in adult patients 18 years of age and older with active non-radiographic axial spondyloarthritis. Patients met ASAS criteria for axial spondyloarthritis and had active disease as defined by a BASDAI greater or equal to 4, a Visual Analogue Scale (VAS) for total back pain greater or equal to 40 (on a scale of 0-100 mm) despite NSAID therapy and no evidence of radiographic changes in the sacroiliac joints that would meet the modified New York criteria for AS. Patients also had to have objective signs of inflammation with a C-reactive protein (CRP) level above the upper limit of normal and/or evidence of sacroiliitis on Magnetic Resonance Imaging (MRI). Approximately 10% and 15% of patients used concomitant methotrexate or sulfasalazine, respectively. Overall, 10% of patients had received previous treatment with anti-TNFα agents and discontinued these due to either lack of efficacy or intolerance.
Patients were treated with COSENTYX 150 mg subcutaneous treatment with load (Weeks 0, 1, 2, 3, and 4) or without a load (Weeks 0 and 4) followed by the same dose every 4 weeks or placebo. In the double-blind period, patients (n = 555) received either placebo or COSENTYX for 52 weeks. Starting Week 16, dose adjustment or addition of concomitant NSAIDs and DMARDs was permitted. Starting at Week 20, patients were allowed to switch to open-label COSENTYX 150 mg monthly or other biologic at the discretion of the investigator and patient. The primary endpoint was at least 40% improvement in Assessment of Spondyloarthritis International Society (ASAS40) at Week 52.
Clinical Response
In nr-axSpA1 Study, treatment with COSENTYX 150 mg resulted in significant improvements in the measure of disease activity compared to placebo at Week 16 and Week 52 (Table 11).
| Difference in proportions with 95% CI based on normal approximation. | |||||
| Number of subjects with ASAS40 response (%) | COSENTYX 150 mg without load (n = 184) | COSENTYX 150 mg with load (n = 185) | Difference from Placebo (95% CI) | ||
| Placebo (n = 186) | COSENTYX 150 mg without load | COSENTYX 150 mg with load | |||
| Week 16 | 75 (41) | 74 (40) | 52 (28) | 13 (3, 22) | 12 (2, 22) |
| Week 52 | 70 (38) | 62 (34) | 36 (19) | 19 (10, 28) | 14 (5, 23) |
The results of the main components of the ASAS40 response criteria are shown in Table 12.
| COSENTYX 150 mg without load (N = 184) | COSENTYX 150 mg with load (N = 185) | Placebo (N = 186) | ||||
| Baseline | Week 16 change from baseline | Baseline | Week 16 change from baseline | Baseline | Week 16 change from baseline | |
| ASAS40 Response criteria | ||||||
| -Patient Global Assessment of Disease Activity (0-100 mm) | 71.0 | -26.2 | 72.6 | -24.1 | 68.8 | -13.8 |
| -Total back pain (0-100 mm) | 72.0 | -25.5 | 73.3 | -25.0 | 70.9 | -15.6 |
| -BASFI (0-10) | 5.9 | -1.6 | 6.2 | -1.8 | 5.9 | -1.0 |
| -Inflammation (0-10) | 6.8 | -2.8 | 7.2 | -2.8 | 6.6 | -1.7 |
| hsCRP (mg/L) Mean Change at Week 16 | 9.8 | -4.7 | 13.4 | -7.9 | 9.2 | -2.4 |
| BASDAI (0-10) | 6.9 | -2.4 | 7.1 | -2.4 | 6.8 | -1.5 |
| -Spinal Pain | 7.6 | -3.0 | 7.8 | -3.0 | 7.5 | -2.0 |
| -Peripheral pain and swelling (0-10) | 6.6 | -2.4 | 6.3 | -2.3 | 6.1 | -1.6 |
| BASMI | 2.8 | -0.3 | 2.9 | -0.3 | 2.8 | -0.1 |
The percentage of patients achieving an ASAS40 response by visit is shown in Figure 4.
Figure 4: ASAS40 Responses in nr-axSpA1 Study Over Time up to Week 16
Health Related Quality of Life
COSENTYX treated patients showed improvement in both load and without load arms compared to placebo-treated patients at Week 16 in health-related quality of life as measured by ASQoL (LS mean change: Week 16: -3.5 and -3.6 vs -1.8, respectively).
16.1 How Supplied
COSENTYX (secukinumab) injection is a clear to opalescent, colorless to slightly yellowish solution available as follows:
COSENTYX Sensoready pen:
- NDC 0078-0639-41: Carton of two 150 mg/mL (300 mg dose) single-dose Sensoready pens (injection)
- NDC 0078-0639-68: Carton of one 150 mg/mL single-dose Sensoready pen (injection)
- NDC 0078-0639-98: Carton of two 150 mg/mL (300 mg dose) single-dose prefilled syringes (injection)
- NDC 0078-0639-97: Carton of one 150 mg/mL single-dose prefilled syringe (injection)
- NDC 0078-1056-97: Carton of one 75 mg/0.5 mL single-dose prefilled syringe (injection)
- NDC 0078-0657-61: Carton of one 150 mg lyophilized powder in a single-dose vial (for injection)
COSENTYX prefilled syringe:
COSENTYX prefilled syringe (for pediatric patients less than 50 kg):
The removable cap of the COSENTYX 150 mg/mL Sensoready pen and prefilled syringe, and 75 mg/0.5 mL prefilled syringe contains natural rubber latex. Each Sensoready pen and prefilled syringe is equipped with a needle safety guard.
COSENTYX (secukinumab) for injection is a white lyophilized powder for healthcare professional use only available as follows:
16.2 Storage And Handling
Refrigerate COSENTYX Sensoready pens, prefilled syringes, and vials at 2°C to 8°C (36°F to 46°F). Keep the product in the original carton to protect from light until the time of use. Do not freeze. To avoid foaming do not shake. COSENTYX does not contain a preservative; discard any unused portion.
If necessary, COSENTYX Sensoready pens and 150 mg/mL prefilled syringes may be stored for up to 4 days at room temperature not to exceed 30°C (86°F). Write the date COSENTYX was removed from the refrigerator in the space provided on the carton. If unused and not stored above 30°C (86°F), COSENTYX Sensoready pens and 150 mg/mL prefilled syringes may be returned to the refrigerator. Throw away COSENTYX if it has been kept outside of the refrigerator and not been used in over 4 days.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Infections
Inform patients that COSENTYX may lower the ability of their immune system to fight infections. Instruct patients of the importance of communicating any history of infections to the doctor and contacting their doctor if they develop any symptoms of infection [see Warnings and Precautions (5.1)].
Hypersensitivity
Advise patients to seek immediate medical attention if they experience any symptoms of serious hypersensitivity reactions [see Warnings and Precautions (5.4)].
Risk of Hypersensitivity in Latex-Sensitive Individuals
Advise latex-sensitive patients that the removal caps of the COSENTYX Sensoready pen and the COSENTYX 1 mL and 0.5 mL prefilled syringes contain natural rubber latex, which may cause an allergic reaction in latex-sensitive individuals [see Warnings and Precautions (5.5)].
Immunization
Advise patients that vaccination with live vaccines is not recommended during COSENTYX treatment. Instruct patients to inform the healthcare practitioner that they are taking COSENTYX prior to a potential vaccination [see Warnings and Precautions (5.6)].
Instructions on Injection Technique
If a patient or caregiver is to administer COSENTYX using the Sensoready pen or the prefilled syringe, instruct him/her in injection techniques and assess their ability to inject subcutaneously to ensure the proper administration of COSENTYX [see Dosage and Administration (2.6), Medication Guide and Instructions for Use].
For pediatric patients, inform patients and caregivers that pediatric patients should not self-administer COSENTYX using the pre-filled syringe or the Sensoready pen.
Instruct patients or caregivers in the technique of proper syringe and needle disposal, and advise them not to reuse these items. Instruct patients to inject the full amount of COSENTYX according to the directions provided in the Medication Guide and Instructions for Use.
Manufactured by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
US License Number 1244
© Novartis
T2021-66
Principal Display Panel
NDC 0078-0639-97
Cosentyx®
(secukinumab)
Injection
Single-use Prefilled Syringe
150 mg/mL
1 Prefilled Syringe
ATTENTION: Dispense with enclosed Medication Guide.
For Subcutaneous Use Only
Sterile Solution - Contains No Preservative
Caution: Contains Natural Rubber Latex Which May Cause Allergic Reaction.
Rx only
NOVARTIS
NDC 0078-1056-97
Rx only
Cosentyx®
(secukinumab)
Injection
75 mg/0.5 mL
1 Single-dose Prefilled Syringe
For Subcutaneous Use Only
Caution: Contains Natural Rubber Latex
Which May Cause Allergic Reaction.
ATTENTION:
Dispense with enclosed Medication Guide.
NOVARTIS
* Please review the disclaimer below.