FDA Label for Niacin
View Indications, Usage & Precautions
- 1 INDICATIONS AND USAGE
- 2 DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 MORTALITY AND CORONARY HEART DISEASE MORBIDITY
- 5.2 SKELETAL MUSCLE
- 5.3 LIVER DYSFUNCTION
- 5.4 LABORATORY ABNORMALITIES
- 6 ADVERSE REACTIONS
- 6.1 CLINICAL STUDIES EXPERIENCE
- 6.2 POSTMARKETING EXPERIENCE
- 7.1 STATINS
- 7.2 BILE ACID SEQUESTRANTS
- 7.3 ASPIRIN
- 7.4 ANTIHYPERTENSIVE THERAPY
- 7.5 OTHER
- 7.6 LABORATORY TEST INTERACTIONS
- 8.1 PREGNANCY
- 8.3 NURSING MOTHERS
- 8.4 PEDIATRIC USE
- 8.5 GERIATRIC USE
- 8.6 RENAL IMPAIRMENT
- 8.7 HEPATIC IMPAIRMENT
- 8.8 GENDER
- 10 OVERDOSAGE
- 11 DESCRIPTION
- 12.1 MECHANISM OF ACTION
- 12.3 PHARMACOKINETICS
- 13.1 CARCINOGENESIS AND MUTAGENESIS AND IMPAIRMENT OF FERTILITY
- 14.1 NIACIN CLINICAL STUDIES
- 14.2 NIACIN EXTENDED-RELEASE CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17.1 PATIENT COUNSELING
Niacin Product Label
The following document was submitted to the FDA by the labeler of this product Marlex Pharmaceuticals Inc. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
1 Indications And Usage
Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in individuals at significantly increased risk for atherosclerotic vascular disease due to hyperlipidemia. Niacin therapy is indicated as an adjunct to diet when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate.
- Niacin extended-release tablets are indicated to reduce elevated TC, LDL-C, Apo B and TG levels, and to increase HDL-C in patients with primary hyperlipidemia and mixed dyslipidemia.
- In patients with a history of myocardial infarction and hyperlipidemia, niacin is indicated to reduce the risk of recurrent nonfatal myocardial infarction.
- In patients with a history of coronary artery disease (CAD) and hyperlipidemia, niacin, in combination with a bile acid binding resin, is indicated to slow progression or promote regression of atherosclerotic disease.
- Niacin extended-release tablets in combination with a bile acid binding resin is indicated to reduce elevated TC and LDL-C levels in adult patients with primary hyperlipidemia.
- Niacin is also indicated as adjunctive therapy for treatment of adult patients with severe hypertriglyceridemia who present a risk of pancreatitis and who do not respond adequately to a determined dietary effort to control them.
Limitations of Use
Addition of niacin extended-release tablets did not reduce cardiovascular morbidity or mortality among patients treated with simvastatin in a large, randomized controlled trial (AIM-HIGH) [see Warnings and Precautions (5.1)].
2 Dosage And Administration
Niacin extended-release tablets should be taken at bedtime, after a low-fat snack, and doses should be individualized according to patient response. Therapy with niacin extended-release tablets must be initiated at 500 mg at bedtime in order to reduce the incidence and severity of side effects which may occur during early therapy. The recommended dose escalation is shown in Table 1 below.
| Week(s) | Daily dose | Niacin Extended- Release Tablets Dosage | |
| INITIAL TITRATION | 1 to 4 | 500mg | 1 Niacin Extended-Release Tablet 500mg at bedtime |
| SCHEDULE | 5 to 8 | 1000mg | 1 Niacin Extended-Release Tablet 1000mg or 2 Niacin Extended-Release Tablets 500mg at bedtime |
| * | 1500mg | 3 Niacin Extended-Release Tablets 500mg at bedtime | |
| * | 2000mg | 2 Niacin Extended-Release Tablets 1000mg or 4 Niacin Extended Release Tablets 500mg at bedtime | |
| * After Week 8, titrate to patient response and tolerance. If response to 1000 mg daily is inadequate, increase dose to 1500 mg daily; may subsequently increase dose to 2000 mg daily. Daily dose should not be increased more than 500 mg in a 4-week period, and doses above 2000 mg daily are not recommended. Women may respond at lower doses than men. | |||
Maintenance Dose
The daily dosage of niacin extended-release tablets should not be increased by more than 500 mg in any 4–week period. The recommended maintenance dose is 1000 mg (two 500 mg tablets or one 1000 mg tablet) to 2000 mg (two 1000 mg tablets or four 500 mg tablets) once daily at bedtime. Doses greater than 2000 mg daily are not recommended. Women may respond at lower niacin extended-release tablets doses than men [see Clinical Studies (14.2)].
Single-dose bioavailability studies have demonstrated that two of the 500 mg and one of the 1000 mg tablet strengths are interchangeable but three of the 500 mg and two of the 750 mg tablet strengths are not interchangeable.
Tolerance to flushing develops rapidly over the course of several weeks. Flushing, pruritus, and gastrointestinal distress are also greatly reduced by slowly increasing the dose of niacin and avoiding administration on an empty stomach. Concomitant alcoholic, hot drinks or spicy foods may increase the side effects of flushing and pruritus and should be avoided around the time of niacin extended-release tablets ingestion.
Equivalent doses of niacin extended-release tablets should not be substituted for sustained-release (modified-release, timed-release) niacin preparations or immediate-release (crystalline) niacin [see Warnings and Precautions (5)]. Patients previously receiving other niacin products should be started with the recommended niacin extended-release tablets titration schedule (see Table 1), and the dose should subsequently be individualized based on patient response.
If niacin extended-release tablets therapy is discontinued for an extended period, reinstitution of therapy should include a titration phase (see Table 1).
Niacin extended-release tablets should be taken whole and should not be broken, crushed or chewed before swallowing.
Dosage in Patients with Renal or Hepatic Impairment
Use of niacin extended-release tablets in patients with renal or hepatic impairment has not been studied. Niacin extended-release tablets are contraindicated in patients with significant or unexplained hepatic dysfunction. Niacin extended-release tablets should be used with caution in patients with renal impairment [see Warnings and Precautions (5)].
3 Dosage Forms And Strengths
- 500 mg light orange to orange colored, round shaped, film-coated tablets debossed with ‘AN 321’ on one side and plain on the other side.
- 750 mg light brown to brown colored, capsule shaped, film-coated tablets debossed with ‘AN 322’ on one side and plain on the other side.
- 1000 mg light orange to orange colored, capsule shaped, film-coated tablets debossed with ‘AN 323’ on one side and plain on the other side
4 Contraindications
Niacin extended-release tablets are contraindicated in the following conditions:
- Active liver disease or unexplained persistent elevations in hepatic transaminases [see Warnings and Precautions (5.3)]
- Patients with active peptic ulcer disease
- Patients with arterial bleeding
- Hypersensitivity to niacin or any component of this medication [see Adverse Reactions (6.1)]
5 Warnings And Precautions
Niacin extended-release preparations should not be substituted for equivalent doses of immediate-release (crystalline) niacin. For patients switching from immediate-release niacin to niacin extended-release, therapy with niacin extended-release should be initiated with low doses (i.e., 500 mg at bedtime) and the niacin extended-release dose should then be titrated to the desired therapeutic response [see Dosage and Administration (2)].
Caution should also be used when niacin is used in patients with unstable angina or in the acute phase of an MI, particularly when such patients are also receiving vasoactive drugs such as nitrates, calcium channel blockers, or adrenergic blocking agents.
Niacin is rapidly metabolized by the liver, and excreted through the kidneys. Niacin is contraindicated in patients with significant or unexplained hepatic impairment [see Contraindications (4) and Warnings and Precautions (5.3)] and should be used with caution in patients with renal impairment. Patients with a past history of jaundice, hepatobiliary disease, or peptic ulcer should be observed closely during niacin therapy.
5.1 Mortality And Coronary Heart Disease Morbidity
Niacin extended-release has not been shown to reduce cardiovascular morbidity or mortality among patients already treated with a statin.
The Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglycerides:
Impact on Global Health Outcomes (AIM-HIGH) trial was a randomized placebo-controlled trial of 3414 patients with stable, previously diagnosed cardiovascular disease. Mean baseline lipid levels were LDL-C 74 mg/dL, HDL-C 35 mg/dL, non-HDL-C 111 mg/dL and median triglyceride level of 163 to 177 mg/dL. Ninety-four percent of patients were on background statin therapy prior to entering the trial. All participants received simvastatin, 40 to 80 mg per day, plus ezetimibe 10 mg per day if needed, to maintain an LDL-C level of 40 to 80 mg/dL, and were randomized to receive niacin extended-release 1500 to 2000 mg/day (n=1718) or matching placebo (IR Niacin, 100 to 150 mg, n=1696). On-treatment lipid changes at two years for LDL-C were -12% for the simvastatin plus niacin extended-release group and -5.5% for the simvastatin plus placebo group. HDL-C increased by 25% to 42 mg/dL in the simvastatin plus niacin extended-release group and by 9.8% to 38 mg/dL in the simvastatin plus placebo group (P<0.001). Triglyceride levels decreased by 28.6% in the simvastatin plus niacin extended-release group and by 8.1% in the simvastatin plus placebo group. The primary outcome was an ITT composite of the first study occurrence of coronary heart disease death, nonfatal myocardial infarction, ischemic stroke, hospitalization for acute coronary syndrome or symptom-driven coronary or cerebral revascularization procedures. The trial was stopped after a mean follow-up period of 3 years owing to a lack of efficacy. The primary outcome occurred in 282 patients in the simvastatin plus niacin extended-release group (16.4%) and in 274 patients in the simvastatin plus placebo group (16.2%) (HR 1.02 [95% CI, 0.87 to 1.21], P=0.79. In an ITT analysis, there were 42 cases of first occurrence of ischemic stroke reported, 27 (1.6%) in the simvastatin plus niacin extended-release group and 15 (0.9%) in the simvastatin plus placebo group, a non-statistically significant result (HR 1.79, [95%CI = 0.95 to 3.36], p=0.071). The on-treatment ischemic stroke events were 19 for the simvastatin plus niacin extended-release group and 15 for the simvastatin plus placebo group [see Adverse Reactions (6.1)].
5.2 Skeletal Muscle
Cases of rhabdomyolysis have been associated with concomitant administration of lipid-altering doses (≥1 g/day) of niacin and statins. Elderly patients and patients with diabetes, renal failure, or uncontrolled hypothyroidism are particularly at risk. Monitor patients for any signs and symptoms of muscle pain, tenderness, or weakness, particularly during the initial months of therapy and during any periods of upward dosage titration. Periodic serum creatine phosphokinase (CPK) and potassium determinations should be considered in such situations, but there is no assurance that such monitoring will prevent the occurrence of severe myopathy.
5.3 Liver Dysfunction
Cases of severe hepatic toxicity, including fulminant hepatic necrosis, have occurred in patients who have substituted sustained-release (modified-release, timed-release) niacin products for immediate-release (crystalline) niacin at equivalent doses.
Niacin extended-release should be used with caution in patients who consume substantial quantities of alcohol and/or have a past history of liver disease. Active liver diseases or unexplained transaminase elevations are contraindications to the use of niacin extended-release.
Niacin preparations have been associated with abnormal liver tests. In three placebo-controlled clinical trials involving titration to final daily niacin extended-release doses ranging from 500 to 3000 mg, 245 patients received niacin extended-release for a mean duration of 17 weeks. No patient with normal serum transaminase levels (AST, ALT) at baseline experienced elevations to more than 3 times the upper limit of normal (ULN) during treatment with niacin extended-release. In these studies, fewer than 1% (2/245) of niacin extended-release patients discontinued due to transaminase elevations greater than 2 times the ULN.
Liver-related tests should be performed on all patients during therapy with niacin extended-release.
Serum transaminase levels, including AST and ALT (SGOT and SGPT), should be monitored before treatment begins, every 6 to 12 weeks for the first year, and periodically thereafter (e.g., at approximately 6-month intervals). Special attention should be paid to patients who develop elevated serum transaminase levels, and in these patients, measurements should be repeated promptly and then performed more frequently. If the transaminase levels show evidence of progression, particularly if they rise to 3 times ULN and are persistent, or if they are associated with symptoms of nausea, fever, and/or malaise, the drug should be discontinued.
5.4 Laboratory Abnormalities
Increase in Blood Glucose: Niacin treatment can increase fasting blood glucose. Frequent monitoring of blood glucose should be performed to ascertain that the drug is producing no adverse effects. Diabetic patients may experience a dose-related increase in glucose intolerance. Diabetic or potentially diabetic patients should be observed closely during treatment with niacin extended-release, particularly during the first few months of use or dose adjustment; adjustment of diet and/or hypoglycemic therapy may be necessary.
Reduction in platelet count: Niacin extended-release has been associated with small but statistically significant dose-related reductions in platelet count (mean of -11% with 2000 mg). Caution should be observed when niacin extended-release is administered concomitantly with anticoagulants; platelet counts should be monitored closely in such patients.
Increase in Prothrombin Time (PT): Niacin extended-release has been associated with small but statistically significant increases in prothrombin time (mean of approximately +4%); accordingly, patients undergoing surgery should be carefully evaluated. Caution should be observed when niacin extended-release is administered concomitantly with anticoagulants; prothrombin time should be monitored closely in such patients.
Increase in Uric Acid: Elevated uric acid levels have occurred with niacin therapy, therefore use with caution in patients predisposed to gout.
Decrease in Phosphorus: In placebo-controlled trials, niacin extended-release has been associated with small but statistically significant, dose-related reductions in phosphorus levels (mean of -13% with 2000 mg). Although these reductions were transient, phosphorus levels should be monitored periodically in patients at risk for hypophosphatemia.
6 Adverse Reactions
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
6.1 Clinical Studies Experience
In the placebo-controlled clinical trials database of 402 patients (age range 21 to 75 years, 33% women, 89% Caucasians, 7% Blacks, 3% Hispanics, 1% Asians) with a median treatment duration of 16 weeks, 16% of patients on niacin extended-release and 4% of patients on placebo discontinued due to adverse reactions. The most common adverse reactions in the group of patients treated with niacin extended-release that led to treatment discontinuation and occurred at a rate greater than placebo were flushing (6% vs. 0%), rash (2% vs. 0%), diarrhea (2% vs. 0%), nausea (1% vs. 0%), and vomiting (1% vs. 0%). The most commonly reported adverse reactions (incidence >5% and greater than placebo) in the niacin extended-release controlled clinical trial database of 402 patients were flushing, diarrhea, nausea, vomiting, increased cough and pruritus.
In the placebo-controlled clinical trials, flushing episodes (i.e., warmth, redness, itching and/or tingling) were the most common treatment-emergent adverse reactions (reported by as many as 88% of patients) for niacin extended-release. Spontaneous reports suggest that flushing may also be accompanied by symptoms of dizziness, tachycardia, palpitations, shortness of breath, sweating, burning sensation/skin burning sensation, chills, and/or edema, which in rare cases may lead to syncope. In pivotal studies, 6% (14/245) of niacin extended-release patients discontinued due to flushing. In comparisons of immediate-release (IR) niacin and niacin extended-release tablets, although the proportion of patients who flushed was similar, fewer flushing episodes were reported by patients who received niacin extended-release. Following 4 weeks of maintenance therapy at daily doses of 1500 mg, the incidence of flushing over the 4-week period averaged 8.6 events per patient for IR niacin versus 1.9 following niacin extended-release.
Other adverse reactions occurring in ≥5% of patients treated with niacin extended-release and at an incidence greater than placebo are shown in Table 2 below.
| Placebo-Controlled Studies Niacin Extended-Release Treatment@ | |||||
| Recommended Daily Maintenance Doses † | |||||
| Placebo (n=157) | 500 mg ‡ (n=87) | 1000 mg (n=110) | 1500 mg (n=136) | 2000 mg (n=95) | |
| % | % | % | % | % | |
| Gastrointestinal Disorders | |||||
| Diarrhea | 13 | 7 | 10 | 10 | 14 |
| Nausea | 7 | 5 | 6 | 4 | 11 |
| Vomiting | 4 | 0 | 2 | 4 | 9 |
| Respiratory | |||||
| Cough, Increased | 6 | 3 | |||
| Skin and Subcutaneous Tissue Disorders | |||||
| Pruritus | 2 | 8 | 0 | 3 | 0 |
| Rash | 0 | 5 | 5 | 5 | 0 |
| Vascular Disorders | |||||
| Flushing& | 19 | 68 | 69 | 63 | 55 |
| Note: Percentages are calculated from the total number of patients in each column. †Adverse reactions are reported at the initial dose where they occur. @Pooled results from placebo-controlled studies; for niacin extended-release, n = 245 and median treatment duration = 16 weeks. Number of niacin patients (n) are not additive across doses. ‡The 500 mg/day dose is outside the recommended daily maintenance dosing range [see Dosage and Administration (2)]. &10 patients discontinued before receiving 500 mg, therefore they were not included. | |||||
In general, the incidence of adverse events was higher in women compared to men.
Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglycerides:
Impact on Global Health Outcomes (AIM-HIGH)
In AIM-HIGH involving 3414 patients (mean age of 64 years, 15% women, 92% Caucasians, 34% with diabetes mellitus) with stable, previously diagnosed cardiovascular disease, all patients received simvastatin, 40 to 80 mg per day, plus ezetimibe 10 mg per day if needed, to maintain an LDL-C level of 40 to 80 mg/dL, and were randomized to receive niacin extended-release 1500 to 2000 mg/day (n=1718) or matching placebo (IR Niacin, 100 to 150 mg, n=1696). The incidence of the adverse reactions of “blood glucose increased” (6.4% vs. 4.5%) and “diabetes mellitus” (3.6% vs. 2.2%) was significantly higher in the simvastatin plus niacin extended-release group as compared to the simvastatin plus placebo group. There were 5 cases of rhabdomyolysis reported, 4 (0.2%) in the simvastatin plus niacin extended-release group and one (<0.1%) in the simvastatin plus placebo group [see Warnings and Precautions (5.1)].
6.2 Postmarketing Experience
Because the below reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following additional adverse reactions have been identified during post-approval use of niacin extended-release:
Hypersensitivity reactions, including anaphylaxis, angioedema, urticaria, flushing, dyspnea, tongue edema, larynx edema, face edema, peripheral edema, laryngismus, and vesiculobullous rash; maculopapular rash; dry skin; tachycardia; palpitations; atrial fibrillation; other cardiac arrhythmias; syncope; hypotension; postural hypotension; blurred vision; macular edema; peptic ulcers; eructation; flatulence; hepatitis; jaundice; decreased glucose tolerance; gout; myalgia; myopathy; dizziness; insomnia; asthenia; nervousness; paresthesia; dyspnea; sweating; burning sensation/skin burning sensation; skin discoloration, and migraine.
Clinical Laboratory Abnormalities
Chemistry: Elevations in serum transaminases [see Warnings and Precautions (5.3)], LDH, fasting glucose, uric acid, total bilirubin, amylase and creatine kinase, and reduction in phosphorus.
Hematology: Slight reductions in platelet counts and prolongation in prothrombin time [see Warnings and Precautions (5.4)].
7.1 Statins
Caution should be used when prescribing niacin (≥1 gm/day) with statins as these drugs can increase risk of myopathy/rhabdomyolysis [see Warnings and Precautions (5) and Clinical Pharmacology (12.3)].
7.2 Bile Acid Sequestrants
An in vitro study results suggest that the bile acid-binding resins have high niacin binding capacity.
Therefore, 4 to 6 hours, or as great an interval as possible, should elapse between the ingestion of bile acid-binding resins and the administration of niacin extended-release [see Clinical Pharmacology (12.3)].
7.3 Aspirin
Concomitant aspirin may decrease the metabolic clearance of nicotinic acid. The clinical relevance of this finding is unclear.
7.4 Antihypertensive Therapy
Niacin may potentiate the effects of ganglionic blocking agents and vasoactive drugs resulting in postural hypotension.
7.5 Other
Vitamins or other nutritional supplements containing large doses of niacin or related compounds such as nicotinamide may potentiate the adverse effects of niacin extended-release.
7.6 Laboratory Test Interactions
Niacin may produce false elevations in some fluorometric determinations of plasma or urinary catecholamines. Niacin may also give false-positive reactions with cupric sulfate solution (Benedict’s reagent) in urine glucose tests.
8.1 Pregnancy
Pregnancy Category C.
Animal reproduction studies have not been conducted with niacin or with niacin extended-release. It is also not known whether niacin at doses typically used for lipid disorders can cause fetal harm when administered to pregnant women or whether it can affect reproductive capacity. If a woman receiving niacin for primary hyperlipidemia becomes pregnant, the drug should be discontinued. If a woman being treated with niacin for hypertriglyceridemia conceives, the benefits and risks of continued therapy should be assessed on an individual basis.
8.3 Nursing Mothers
Niacin is excreted into human milk but the actual infant dose or infant dose as a percent of the maternal dose is not known. Because of the potential for serious adverse reactions in nursing infants from lipidaltering doses of nicotinic acid, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. No studies have been conducted with niacin extended-release in nursing mothers.
8.4 Pediatric Use
Safety and effectiveness of niacin therapy in pediatric patients (≤16 years) have not been established.
8.5 Geriatric Use
Of 979 patients in clinical studies of niacin extended-release, 21% of the patients were age 65 and over.
No overall differences in safety and effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
No studies have been performed in this population. Niacin extended-release should be used with caution in patients with renal impairment [see Warnings and Precautions (5)].
8.7 Hepatic Impairment
No studies have been performed in this population. Niacin extended-release should be used with caution in patients with a past history of liver disease and/or who consume substantial quantities of alcohol. Active liver disease, unexplained transaminase elevations and significant or unexplained hepatic dysfunction are contraindications to the use of niacin extended-release [see Contraindications (4.0) and Warnings and Precautions (5.3)].
8.8 Gender
Data from the clinical trials suggest that women have a greater hypolipidemic response than men at equivalent doses of niacin extended-release.
10 Overdosage
Supportive measures should be undertaken in the event of an overdose.
11 Description
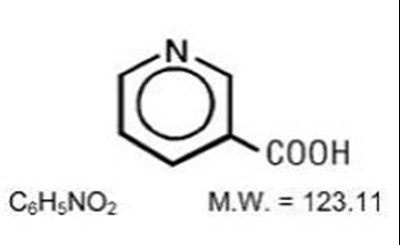
Niacin extended-release tablets contains niacin, USP, which at therapeutic doses is an antihyperlipidemic agent. Niacin, USP (nicotinic acid, or 3-pyridinecarboxylic acid) is a white, crystalline powder, very soluble in water, with the following structural formula:
Niacin extended-release tablets are unscored, film-coated tablets for oral administration and are available in two tablet strengths containing 500 mg and 1000 mg niacin. The 500 mg is light orange to orange colored, round shaped, coated tablets debossed with ‘AN 321’ on one side and plain on the other side. The 1000 mg is light orange to orange colored, capsule shaped, coated tablets debossed with ‘AN 323’ on one side and plain on the other side. Niacin extended-release tablets also contain the following inactive ingredients: FD&C yellow #6/sunset yellow FCF aluminum lake, hydroxyethyl cellulose, hypromellose, iron oxide red, iron oxide yellow, polyethylene glycol 400, stearic acid and titanium dioxide.
12.1 Mechanism Of Action
The mechanism by which niacin alters lipid profiles has not been well defined. It may involve several actions including partial inhibition of release of free fatty acids from adipose tissue, and increased lipoprotein lipase activity, which may increase the rate of chylomicron triglyceride removal from plasma. Niacin decreases the rate of hepatic synthesis of VLDL and LDL, and does not appear to affect fecal excretion of fats, sterols, or bile acids.
12.3 Pharmacokinetics
Absorption
Due to extensive and saturable first-pass metabolism, niacin concentrations in the general circulation are dose dependent and highly variable. Time to reach the maximum niacin plasma concentrations was about 5 hours following niacin extended-release. To reduce the risk of gastrointestinal (GI) upset, administration of niacin extended-release with a low-fat meal or snack is recommended.
Single-dose bioavailability studies have demonstrated that the 500 mg and 1000 mg tablet strengths are dosage form equivalent but the 500 mg and 750 mg tablet strengths are not dosage form equivalent.
Metabolism
The pharmacokinetic profile of niacin is complicated due to extensive first-pass metabolism that is dose-rate specific and, at the doses used to treat dyslipidemia, saturable. In humans, one pathway is through a simple conjugation step with glycine to form nicotinuric acid (NUA). NUA is then excreted in the urine, although there may be a small amount of reversible metabolism back to niacin. The other pathway results in the formation of nicotinamide adenine dinucleotide (NAD). It is unclear whether nicotinamide is formed as a precursor to, or following the synthesis of, NAD. Nicotinamide is further metabolized to at least N-methylnicotinamide (MNA) and nicotinamide-N-oxide (NNO). MNA is further metabolized to two other compounds, N-methyl-2-pyridone-5-carboxamide (2PY) and N-methyl-4- pyridone-5-carboxamide (4PY). The formation of 2PY appears to predominate over 4PY in humans. At the doses used to treat hyperlipidemia, these metabolic pathways are saturable, which explains the nonlinear relationship between niacin dose and plasma concentrations following multiple-dose niacin extended-release administration.
Nicotinamide does not have hypolipidemic activity; the activity of the other metabolites is unknown.
Elimination
Following single and multiple doses, approximately 60% to 76% of the niacin dose administered as niacin extended-release was recovered in urine as niacin and metabolites; up to 12% was recovered as unchanged niacin after multiple dosing. The ratio of metabolites recovered in the urine was dependent on the dose administered.
Pediatric Use
No pharmacokinetic studies have been performed in this population (≤16 years) [see Use in Specific Populations (8.4)].
Geriatric Use
No pharmacokinetic studies have been performed in this population (> 65 years) [see Use in Specific Populations (8.5)].
Renal Impairment
No pharmacokinetic studies have been performed in this population. Niacin extended-release should be used with caution in patients with renal disease [see Warnings and Precautions (5)].
Hepatic Impairment
No pharmacokinetic studies have been performed in this population. Active liver disease, unexplained transaminase elevations and significant or unexplained hepatic dysfunction are contraindications to the use of niacin extended-release [see Contraindications (4) and Warnings and Precautions (5.3)].
Gender
Steady-state plasma concentrations of niacin and metabolites after administration of niacin extended-release are generally higher in women than in men, with the magnitude of the difference varying with dose and metabolite. This gender differences observed in plasma levels of niacin and its metabolites may be due to gender-specific differences in metabolic rate or volume of distribution. Recovery of niacin and metabolites in urine, however, is generally similar for men and women, indicating that absorption is similar for both genders [see Gender (8.8)].
Drug interactions
Fluvastatin
Niacin did not affect fluvastatin pharmacokinetics [see Drug Interactions (7.1)].
Lovastatin
When niacin extended-release 2000 mg and lovastatin 40 mg were co-administered, niacin extended-release increased lovastatin Cmax and AUC by 2% and 14%, respectively, and decreased lovastatin acid Cmax and AUC by 22% and 2%, respectively. Lovastatin reduced niacin extended-release bioavailability by 2% to 3% [see Drug Interactions (7.1)].
Simvastatin
When niacin extended-release 2000 mg and simvastatin 40 mg were co-administered, niacin extended-release increased simvastatin Cmax and AUC by 1% and 9%, respectively, and simvastatin acid Cmax and AUC by 2% and 18%, respectively. Simvastatin reduced niacin extended-release bioavailability by 2% [see Drug Interactions (7.1)].
Bile Acid Sequestrants
An in vitro study was carried out investigating the niacin-binding capacity of colestipol and cholestyramine. About 98% of available niacin was bound to colestipol, with 10% to 30% binding to cholestyramine [see Drug Interactions (7.2)].
13.1 Carcinogenesis And Mutagenesis And Impairment Of Fertility
Niacin administered to mice for a lifetime as a 1% solution in drinking water was not carcinogenic. The mice in this study received approximately 6 to 8 times a human dose of 3000 mg/day as determined on a mg/m2 basis. Niacin was negative for mutagenicity in the Ames test. No studies on impairment of fertility have been performed. No studies have been conducted with niacin extended-release regarding carcinogenesis, mutagenesis, or impairment of fertility.
14.1 Niacin Clinical Studies
Niacin’s ability to reduce mortality and the risk of definite, nonfatal myocardial infarction (MI) has been assessed in long-term studies. The Coronary Drug Project, completed in 1975, was designed to assess the safety and efficacy of niacin and other lipid-altering drugs in men 30 to 64 years old with a history of MI. Over an observation period of 5 years, niacin treatment was associated with a statistically significant reduction in nonfatal, recurrent MI. The incidence of definite, nonfatal MI was 8.9% for the 1,119 patients randomized to nicotinic acid versus 12.2% for the 2,789 patients who received placebo (p<0.004). Total mortality was similar in the two groups at 5 years (24.4% with nicotinic acid versus 25.4% with placebo; p=N.S.). At the time of a 15-year follow-up, there were 11% (69) fewer deaths in the niacin group compared to the placebo cohort (52% versus 58.2%; p=0.0004). However, mortality at 15 years was not an original endpoint of the Coronary Drug Project. In addition, patients had not received niacin for approximately 9 years, and confounding variables such as concomitant medication use and medical or surgical treatments were not controlled.
The Cholesterol-Lowering Atherosclerosis Study (CLAS) was a randomized, placebo-controlled, angiographic trial testing combined colestipol and niacin therapy in 162 non-smoking males with previous coronary bypass surgery. The primary, per-subject cardiac endpoint was global coronary artery change score. After 2 years, 61% of patients in the placebo cohort showed disease progression by global change score (n=82), compared with only 38.8% of drug-treated subjects (n=80), when both native arteries and grafts were considered (p<0.005); disease regression also occurred more frequently in the drug-treated group (16.2% versus 2.4%; p=0.002). In a follow-up to this trial in a subgroup of 103 patients treated for 4 years, again, significantly fewer patients in the drug-treated group demonstrated progression than in the placebo cohort (48% versus 85%, respectively; p<0.0001).
The Familial Atherosclerosis Treatment Study (FATS) in 146 men ages 62 and younger with Apo B levels ≥125 mg/dL, established coronary artery disease, and family histories of vascular disease, assessed change in severity of disease in the proximal coronary arteries by quantitative arteriography. Patients were given dietary counseling and randomized to treatment with either conventional therapy with double placebo (or placebo plus colestipol if the LDL-C was elevated); lovastatin plus colestipol; or niacin plus colestipol. In the conventional therapy group, 46% of patients had disease progression (and no regression) in at least one of nine proximal coronary segments; regression was the only change in 11%. In contrast, progression (as the only change) was seen in only 25% in the niacin plus colestipol group, while regression was observed in 39%. Though not an original endpoint of the trial, clinical events (death, MI, or revascularization for worsening angina) occurred in 10 of 52 patients who received conventional therapy, compared with 2 of 48 who received niacin plus colestipol.
14.2 Niacin Extended-Release Clinical Studies
Placebo-Controlled Clinical Studies in Patients with Primary Hyperlipidemia and Mixed Dyslipidemia: In two randomized, double-blind, parallel, multi-center, placebo-controlled trials, niacin extended-release dosed at 1000, 1500 or 2000 mg daily at bedtime with a low-fat snack for 16 weeks (including 4 weeks of dose escalation) favorably altered lipid profiles compared to placebo (Table 3). Women appeared to have a greater response than men at each niacin extended-release dose level (see Gender Effect, below).
| Mean Percent Change from Baseline to Week 16* | ||||||
| Treatment | n | TC | LDL-C | HDL-C | TG | Apo B |
| Niacin Extended-Release 1000mg at | 41 | -3 | -5 | +18 | -21 | -6 |
| Bedtime | ||||||
| Niacin Extended-Release 2000mg at | 41 | -10 | -14 | +22 | -28 | -16 |
| Bedtime | ||||||
| Placebo | 40 | 0 | -1 | +4 | 0 | +1 |
| Niacin Extended-Release 1500 mg at | 76 | -8 | -12 | +20 | -13 | -12 |
| Bedtime | ||||||
| Placebo | 73 | +2 | +1 | +2 | +12 | +1 |
| n = number of patients at baseline; * Mean percent change from baseline for all niacin extended-release doses was significantly different (p < 0.05) from placebo. | ||||||
In a double-blind, multi-center, forced dose-escalation study, monthly 500 mg increases in niacin extended-release dose resulted in incremental reductions of approximately 5% in LDL-C and Apo B levels in the daily dose range of 500 mg through 2000 mg (Table 4). Women again tended to have a greater response to niacin extended-release than men (see Gender Effect, below).
| Mean Percent in Dose-Escalation Study | |||||||
| Treatment | n | TC | LDL-C | HDL-C | TG | Apo B | |
| Placebo‡ | 44 | -2 | -1 | +5 | -6 | -2 | |
| Niacin Extended-Release | 87 | ||||||
| 500 mg at bedtime | -2 | -3 | +10 | -5 | -2 | ||
| 1000 mg at bedtime | -5 | -9 | +15 | -11 | -7 | ||
| 1500 mg at bedtime | -11 | -14 | +22 | -28 | -15 | ||
| 2000 mg at bedtime | -12 | -17 | +26 | -35 | -16 | ||
| n = number of patients enrolled; ‡Placebo data shown are after 24 weeks of placebo treatment. * For all niacin extended-release doses except 500 mg, mean percent change from baseline was significantly different (p < 0.05) from placebo for all lipid parameters shown. | |||||||
Pooled results for major lipids from these three placebo-controlled studies are shown below (Table 5).
| Mean Baseline and Median Percent Change from Baseline (25th, 75th Percentiles) | ||||
| Niacin Extended-Release Dose | n | LDL-C | HDL-C | TG |
| 1000 mg at bedtime | 104 | |||
| Baseline (mg/dL) | 218 | 45 | 172 | |
| Percent Change | -7 (-15, 0) | +14 (+7, +23) | -16 (-34, +3) | |
| 1500 mg at bedtime | 120 | |||
| Baseline (mg/dL) | 212 | 46 | 171 | |
| Percent Change | -13 (-21, -4) | +19 (+9, +31) | -25 (-45, -2) | |
| 2000 mg at bedtime | 85 | |||
| Baseline (mg/dL) | 220 | 44 | 160 | |
| Percent Change | -16 (-26, -7) | +22 (+15, +34) | -38 (-52, -14) | |
| * Represents pooled analyses of results; minimum duration on therapy at each dose was 4 weeks. | ||||
Gender Effect: Combined data from the three placebo-controlled niacin extended-release studies in patients with primary hyperlipidemia and mixed dyslipidemia suggest that, at each niacin extended-release dose level studied, changes in lipid concentrations are greater for women than for men (Table 6).
| Mean Percent Change from Baseline | |||||||||
| Niacin Extended-Release | N | LDL-C | HDL-C | TG | Apo B | ||||
| Dose | (M/F) | M | F | M | F | M | F | M | F |
| 500mg at bedtime | 50/37 | -2 | -5 | +11 | +8 | -3 | -9 | -1 | -5 |
| 1000mg at bedtime | 76/52 | -6* | -11* | +14 | +20 | -10 | -20 | -5* | -10* |
| 1500mg at bedtime | 104/59 | -12 | -16 | +19 | +24 | -17 | -28 | -13 | -15 |
| 2000mg at bedtime | 75/53 | -15 | -18 | +23 | +26 | -30 | -36 | -16 | -16 |
| n = number of male/female patients enrolled. * Percent change significantly different between genders (p < 0.05). | |||||||||
Other Patient Populations: In a double-blind, multi-center, 19-week study the lipid-altering effects of niacin extended-release (forced titration to 2000 mg at bedtime) were compared to baseline in patients whose primary lipid abnormality was a low level of HDL-C (HDL-C ≤40 mg/dL, TG ≤400 mg/dL, and LDL-C ≤160, or <130 mg/dL in the presence of CHD). Results are shown below (Table 7).
| Mean Baseline and Mean Percent Change from Baseline* | ||||||
| n | TC | LDL-C | HDL-C | TG | Apo B† | |
| Baseline | 88 | 190 | 120 | 31 | 194 | 106 |
| (mg/dL) | ||||||
| Week 19 | 71 | -3 | 0 | +26 | -30 | -9 |
| (% Change) | ||||||
| n = number of patients * Mean percent change from baseline was significantly different (p < 0.05) for all lipid parameters shown except LDL-C. †n = 72 at baseline and 69 at week 19. | ||||||
At niacin extended-release 2000 mg/day, median changes from baseline (25th, 75th percentiles) for
LDL-C, HDL-C, and TG were -3% (-14, +12%), +27% (+13, +38%), and -33% (-50, -19%), respectively.
16 How Supplied/Storage And Handling
Niacin extended-release tablets 500 mg are supplied as light orange to orange colored, round shaped, film-coated tablets debossed with “AN 321” on one side and plain on the other side.
They are available as follows:
Bottles of 30: NDC 10135-0612-30
Bottles of 90: NDC 10135-0612-90
Bottles of 500: NDC 10135-0612-05
Niacin extended-release tablets 750 mg are supplied as light brown to brown colored, capsule shaped, film-coated tablets debossed with “AN 322” on one side and plain on the other side.
They are available as follows:
Bottles of 30: NDC 10135-0613-30
Bottles of 90: NDC 10135-0613-90
Bottles of 500: NDC 10135-0613-05
Niacin extended-release tablets 1000 mg are supplied as light orange to orange colored, capsule shaped, film-coated tablets debossed with “AN 323” on one side and plain on the other side.
They are available as follows:
Bottles of 30: NDC 10135-0614-30
Bottles of 90: NDC 10135-0614-90
Bottles of 500: NDC 10135-0614-05
Storage: Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
17.1 Patient Counseling
Patients should be advised to adhere to their National Cholesterol Education Program (NCEP) recommended diet, a regular exercise program, and periodic testing of a fasting lipid panel.
Patients should be advised to inform other healthcare professionals prescribing a new medication that they are taking niacin extended-release.
The patient should be informed of the following:
Dosing Time
Niacin extended-release tablets should be taken at bedtime, after a low-fat snack. Administration on an empty stomach is not recommended.
Tablet Integrity
Niacin extended-release tablets should not be broken, crushed or chewed, but should be swallowed whole.
Dosing Interruption
If dosing is interrupted for any length of time, their physician should be contacted prior to restarting therapy; re-titration is recommended.
Muscle Pain
Notify their physician of any unexplained muscle pain, tenderness, or weakness promptly. They should discuss all medication, both prescription and over the counter, with their physician.
Flushing
Flushing (warmth, redness, itching and/or tingling of the skin) is a common side effect of niacin therapy that may subside after several weeks of consistent niacin extended-release use. Flushing may vary in severity and is more likely to occur with initiation of therapy, or during dose increases. By dosing at bedtime, flushing will most likely occur during sleep. However, if awakened by flushing at night, the patient should get up slowly, especially if feeling dizzy, feeling faint, or taking blood pressure medications. Advise patients of the symptoms of flushing and how they differ from the symptoms of a myocardial infarction.
Diet
Avoid ingestion of alcohol, hot beverages and spicy foods around the time of taking niacin extended-release to minimize flushing.
Supplements
Notify their physician if they are taking vitamins or other nutritional supplements containing niacin or nicotinamide.
Dizziness
Notify their physician if symptoms of dizziness occur.
Diabetics
If diabetic, to notify their physician of changes in blood glucose.
Pregnancy
Discuss future pregnancy plans with your patients, and discuss when to stop niacin extended-release if they are trying to conceive. Patients should be advised that if they become pregnant, they should stop taking niacin extended-release and call their healthcare professional.
Breastfeeding
Women who are breastfeeding should be advised to not use niacin extended-release. Patients, who have a lipid disorder and are breastfeeding, should be advised to discuss the options with their healthcare professional.
Manufactured for and Distributed By:
Marlex Pharmaceuticals, Inc.
New Castle, DE 19720
Rev. 02/16AN
* Please review the disclaimer below.