FDA Label for Riomet
View Indications, Usage & Precautions
- OTHER
- DESCRIPTION
- MECHANISM OF ACTION
- ABSORPTION AND BIOAVAILABILITY
- DISTRIBUTION
- METABOLISM AND ELIMINATION
- PATIENTS WITH TYPE 2 DIABETES
- RENAL IMPAIRMENT
- HEPATIC IMPAIRMENT
- GERIATRICS
- PEDIATRICS
- GENDER
- RACE
- CLINICAL STUDIES
- PEDIATRIC CLINICAL STUDIES
- INDICATION AND USAGE
- CONTRAINDICATIONS
- WARNING: LACTIC ACIDOSIS
- PRECAUTIONS
- ADVERSE REACTIONS
- PEDIATRIC PATIENTS
- OVERDOSAGE
- DOSAGE AND ADMINISTRATION
- RECOMMENDATIONS FOR USE IN RENAL IMPAIRMENT
- DISCONTINUATION FOR IODINATED CONTRAST IMAGING PROCEDURES
- CONCOMITANT METFORMIN AND ORAL SULFONYLUREA THERAPY IN ADULT PATIENTS
- CONCOMITANT METFORMIN AND INSULIN THERAPY IN ADULT PATIENTS
- SPECIFIC PATIENT POPULATIONS
- HOW SUPPLIED
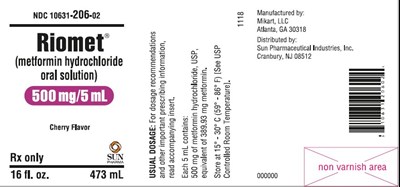
- PACKAGE/LABEL DISPLAY PANEL
Riomet Product Label
The following document was submitted to the FDA by the labeler of this product Sun Pharmaceutical Industries, Inc.. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
Other
Rx only
Adults - The usual starting dose of RIOMET (metformin hydrochloride oral solution) is 500 mg (5 mL) twice a day or 850 mg (8.5 mL) once a day, given with meals. In general, clinically significant responses are not seen at doses below 1500 mg per day. Dosage increases should be made in increments of 500 mg (5 mL) weekly or 850 mg (8.5 mL) every 2 weeks, up to a total of 2000 mg (20 mL) per day, given in divided doses. The dosage of RIOMET must be individualized on the basis of both effectiveness and tolerability. Patients can also be titrated from 500 mg (5 mL) twice a day to 850 mg (8.5 mL) twice a day after 2 weeks. For those patients requiring additional glycemic control, RIOMET may be given to a maximum daily dose of 2550 mg (25.5 mL) per day. Doses above 2000 mg (20 mL) may be better tolerated given three times a day with meals.
Pediatrics - The usual starting dose of RIOMET is 500 mg (5 mL) twice a day, given with meals. Dosage increases should be made in increments of 500 mg (5 mL) weekly up to a maximum of 2000 mg (20 mL) per day, given in divided doses. The dosage of RIOMET must be individualized on the basis of both effectiveness and tolerability.
Description
RIOMET (metformin hydrochloride oral solution) is an oral antihyperglycemic drug used in the management of type 2 diabetes. Metformin hydrochloride, USP (N,N-dimethylimidodicarbonimidic diamide hydrochloride) is not chemically or pharmacologically related to any other classes of oral antihyperglycemic agents. The structural formula is as shown:
Metformin hydrochloride, USP is a white crystalline powder with a molecular formula of C4H11N5•HCl and a molecular weight of 165.62. Metformin hydrochloride, USP 2.0 g is soluble in 20 mL of water. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin hydrochloride is 6.68. It is freely soluble in water; slightly soluble in alcohol; practically insoluble in acetone and in methylene chloride.
RIOMET (Cherry Flavor) contains 500 mg of metformin hydrochloride, USP per 5 mL and the following inactive ingredients: Artificial cherry flavor, hydrochloric acid, potassium bicarbonate, purified water, saccharin calcium, and xylitol.
RIOMET (Strawberry Flavor) contains 500 mg of metformin hydrochloride, USP per 5 mL and the following inactive ingredients: Hydrochloric acid, N&A strawberry flavor (propylene glycol and glycerin), potassium bicarbonate, purified water, sucralose, and xylitol.
Mechanism Of Action
Metformin is an antihyperglycemic agent which improves glucose tolerance in patients with type 2 diabetes, lowering both basal and postprandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral antihyperglycemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Unlike sulfonylureas, metformin does not produce hypoglycemia in either patients with type 2 diabetes or normal subjects (except in special circumstances, see PRECAUTIONS) and does not cause hyperinsulinemia. With metformin therapy, insulin secretion remains unchanged while fasting insulin levels and day-long plasma insulin response may actually decrease.
Absorption And Bioavailability
Two pharmacokinetic studies have been performed in healthy volunteers to evaluate the bioavailability of RIOMET in comparison with the commercially available metformin tablets under fasting and fed conditions (study 1 and study 2). A third pharmacokinetic study (study 3) assessed effects of food on absorption of RIOMET.
The rate and extent of absorption of RIOMET was found to be comparable to that of Metformin tablets under fasting or fed conditions (see Table 1).
| T-test product (RIOMET) | |||
| R-reference product (metformin tablets) | |||
Table 1. Select Mean (± S.D.) Pharmacokinetic Parameters Following Single Oral Doses of 1000 mg RIOMET and Metformin tablets in healthy, nondiabetic adults (n = 36) under fed and fasting conditions | |||
Formulation | Cmax (ng/mL) | AUC0-∞ (ng.h/mL) | tmax (h) |
Study 1- Fasting state | |||
RIOMET | 1540.1 ± 451.1 | 9069.6 ± 2593.6 | 2.2 ± 0.5 |
Metformin Tablets | 1885.1 ± 498.5 | 11100.1 ± 2733.1 | 2.5 ± 0.6 |
T/R Ratio X 100 (90% confidence interval) | 81.2 (76.3 - 86.4) | 81.2 (76.9 - 85.6) | - |
Study 2- Fed State | |||
RIOMET | 1235.3 ± 177.7 | 8950.1 ± 1381.2 | 4.1 ± 0.8 |
Metformin Tablets | 1361 ± 298.8 | 9307.7 ± 1839.8 | 3.7 ± 0.8 |
T/R Ratio X 100 (90% confidence interval) | 91.8 (87.4 - 96.5) | 97.0 (92.9 - 101.2) | - |
Table 2. Select Mean (± S.D.) Metformin Pharmacokinetic Parameters Following Single Oral Doses of 1000 mg RIOMET in healthy, nondiabetic adults (n = 33) under fed (high fat/high calorie meal and low fat/low calorie meal) and fasting conditions (study 3) | |||
Meal type | Cmax (ng/mL) | AUC0-∞ (ng.h/mL) | tmax (h) |
Fasting (F) | 1641.5 ± 551.8 | 9982.9 ± 2544.5 | 2.5 ± 0.9 |
Low fat/ low calorie meal (L) | 1525.8 ± 396.7 | 11542.0 ± 2947.5 | 3.9 ± 0.6 |
High fat/high calorie meal (H) | 1432.5 ± 346.8 | 11184.5 ± 2446.1 | 3.9 ± 0.8 |
L/F Ratio X 100 (90% confidence interval) | 94.6 (84.0 - 106.5) | 115.6 (103.6 - 128.9) | - |
H/F Ratio X 100 (90% confidence interval) | 89.4 (79.4 - 100.6) | 112.6 (100.9 - 125.6) | - |
L/H Ratio X 100 (90% confidence interval) | 105.8 (94.0 - 119.2) | 102.7 (92.0 - 114.6) | - |
Studies using single oral doses of metformin tablet formulations 500 mg to 1500 mg, and 850 mg to 2550 mg, indicate that there is a lack of dose proportionality with increasing doses, which is due to decreased absorption rather than an alteration in elimination.
Distribution
The apparent volume of distribution (V/F) of metformin following single oral doses of metformin 850 mg averaged 654 ± 358 L. Metformin is negligibly bound to plasma proteins, in contrast to sulfonylureas, which are more than 90% protein bound. Metformin partitions into erythrocytes, most likely as a function of time. At usual clinical doses and dosing schedules of metformin, steady state plasma concentrations of metformin are reached within 24 to 48 hours and are generally < 1 µg/mL. During controlled clinical trials of metformin, maximum metformin plasma levels did not exceed 5 µg/mL, even at maximum doses.
Metabolism And Elimination
Intravenous single-dose studies in normal subjects demonstrate that metformin is excreted unchanged in the urine and does not undergo hepatic metabolism (no metabolites have been identified in humans) nor biliary excretion. Renal clearance (see Table 3) is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of metformin elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. In blood, the elimination half-life is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
Patients With Type 2 Diabetes
In the presence of normal renal function, there are no differences between single- or multiple-dose pharmacokinetics of metformin between patients with type 2 diabetes and normal subjects (see Table 3), nor is there any accumulation of metformin in either group at usual clinical doses.
Renal Impairment
In patients with decreased renal function, the plasma and blood half-life of metformin is prolonged and the renal clearance is decreased (see Table 3; also see CONTRAINDICATIONS, WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION).
Hepatic Impairment
No pharmacokinetic studies of metformin have been conducted in patients with hepatic insufficiency.
Geriatrics
Limited data from controlled pharmacokinetic studies of metformin in healthy elderly subjects suggest that total plasma clearance of metformin is decreased, the half-life is prolonged, and Cmax is increased, compared to healthy young subjects. From these data, it appears that the change in metformin pharmacokinetics with aging is primarily accounted for by a change in renal function (see Table 3) (See WARNINGS, PRECAUTIONS and DOSAGE AND ADMINISTRATION.)
| a-All doses given fasting except the first 18 doses of the multiple dose studies | |||
| b-Peak plasma concentration | |||
| c-Time to peak plasma concentration | |||
| d-Combined results (average means) of five studies: mean age 32 years (range 23 - 59 years) | |||
| e-Kinetic study done following dose 19, given fasting | |||
| f-Elderly subjects, mean age 71 years (range 65 - 81 years) | |||
| g-CLcr = creatinine clearance normalized to body surface area of 1.73 m2 | |||
Table 3. Select Mean (± S.D.) Metformin Pharmacokinetic Parameters Following Single or Multiple Oral Doses of Metformin | |||
Subject Groups: Metformin dosea (number of subjects) | Cmaxb(µg/mL) | Tmaxc(hrs) | Renal Clearance (mL/min) |
Healthy, nondiabetic adults: |
|
|
|
500 mg single dose (24) | 1.03 (± 0.33) | 2.75 (± 0.81) | 600 (± 132) |
850 mg single dose (74)d | 1.60 (± 0.38) | 2.64 (± 0.82) | 552 (± 139) |
850 mg three times daily for 19 dosese (9) | 2.01 (± 0.42) | 1.79 (± 0.94) | 642 (± 173) |
Adults with type 2 diabetes: |
|
|
|
850 mg single dose (23) | 1.48 (± 0.5) | 3.32 (± 1.08) | 491 (± 138) |
850 mg three times daily for 19 dosese (9) | 1.90 (± 0.62) | 2.01 (± 1.22) | 550 (± 160) |
Elderlyf, healthy nondiabetic adults: |
|
|
|
850 mg single dose (12) | 2.45 (± 0.70) | 2.71 (± 1.05) | 412 (± 98) |
Renally-impaired adults: |
|
|
|
850 mg single dose |
|
|
|
Mild (CLcrg 61 - 90mL/min) (5) | 1.86 (± 0.52) | 3.20 (± 0.45) | 384 (± 122) |
Moderate (CLcr31 - 60mL/min) (4) | 4.12 (± 1.83) | 3.75 (± 0.50) | 108 (± 57) |
Severe (CLcr10 - 30mL/min) (6) | 3.93 (± 0.92) | 4.01 (± 1.10) | 130 (± 90) |
Pediatrics
After administration of a single oral metformin 500 mg dose with food, geometric mean metformin Cmax and AUC differed less than 5% between pediatric type 2 diabetic patients (12 to 16 years of age) and gender- and weight-matched healthy adults (20 to 45 years of age), all with normal renal function.
Gender
Metformin pharmacokinetic parameters did not differ significantly between normal subjects and patients with type 2 diabetes when analyzed according to gender (males = 19, females = 16). Similarly, in controlled clinical studies in patients with type 2 diabetes, the antihyperglycemic effect of metformin was comparable in males and females.
Race
No studies of metformin pharmacokinetic parameters according to race have been performed. In controlled clinical studies of metformin in patients with type 2 diabetes, the antihyperglycemic effect was comparable in whites (n = 249), blacks (n = 51), and Hispanics (n = 24).
Clinical Studies
In a double-blind, placebo-controlled, multicenter U.S. clinical trial involving obese patients with type 2 diabetes whose hyperglycemia was not adequately controlled with dietary management alone (baseline fasting plasma glucose [FPG] of approximately 240 mg/dL), treatment with metformin (up to 2550 mg/day) for 29 weeks resulted in significant mean net reductions in fasting and postprandial plasma glucose (PPG) and hemoglobin A1c (HbA1c) of 59 mg/dL, 83 mg/dL, and 1.8%, respectively, compared to the placebo group (see Table 4).
| *-All patients on diet therapy at Baseline | |||
| **-Not statistically significant | |||
Table 4. Metformin vs Placebo Summary of Mean Changes from Baseline* in Fasting Plasma Glucose, HbA1c, and Body Weight, at Final Visit (29-week study) | |||
| Metformin (n = 141) | Placebo (n = 145) | p-Value |
FPG (mg/ dL) |
|
|
|
Baseline | 241.5 | 237.7 | NS** |
Change at FINAL VISIT | -53.0 | 6.3 | 0.001 |
Hemoglobin A1c (%) |
|
|
|
Baseline | 8.4 | 8.2 | NS** |
Change at FINAL VISIT | -1.4 | 0.4 | 0.001 |
Body Weight (lbs) |
|
|
|
Baseline | 201.0 | 206.0 | NS** |
Change at FINAL VISIT | -1.4 | -2.4 | NS** |
A 29-week, double-blind, placebo-controlled study of metformin and glyburide, alone and in combination, was conducted in obese patients with type 2 diabetes who had failed to achieve adequate glycemic control while on maximum doses of glyburide (baseline FPG of approximately 250 mg/dL) (see Table 5). Patients randomized to the combination arm started therapy with metformin 500 mg and glyburide 20 mg. At the end of each week of the first four weeks of the trial, these patients had their dosages of metformin increased by 500 mg if they had failed to reach target fasting plasma glucose. After week four, such dosage adjustments were made monthly, although no patient was allowed to exceed metformin 2500 mg. Patients in the metformin only arm (metformin plus placebo) followed the same titration schedule. At the end of the trial, approximately 70% of the patients in the combination group were taking metformin 2000 mg/glyburide 20 mg or metformin 2500 mg/glyburide 20 mg. Patients randomized to continue on glyburide experienced worsening of glycemic control, with mean increases in FPG, PPG, and HbA1c of 14 mg/dL, 3 mg/dL, and 0.2%, respectively. In contrast, those randomized to metformin (up to 2500 mg/day) experienced a slight improvement, with mean reductions in FPG, PPG, and HbA1c of 1 mg/dL, 6 mg/dL, and 0.4%, respectively. The combination of metformin and glyburide was effective in reducing FPG, PPG, and HbA1c levels by 63 mg/dL, 65 mg/dL, and 1.7%, respectively. Compared to results of glyburide treatment alone, the net differences with combination treatment were -77 mg/dL, -68 mg/dL, and -1.9%, respectively (see Table 5).
| * All patients on glyburide, 20 mg/day, at Baseline; | ||||||||||
| **-Not statistically significant | ||||||||||
Table 5. Combined Metformin/Glyburide (Comb) vs Glyburide (Glyb) or Metformin (Met) Monotherapy: Summary of Mean Changes from Baseline* in Fasting Plasma Glucose, HbA1c, and Body Weight, at Final Visit (29-week study) | ||||||||||
|
| p-values | ||||||||
| Comb (n = 213) | Glyb (n = 209) | Met (n = 210) | Glyb vs Comb | Met vs Comb | Met vs Glyb | ||||
Fasting Plasma Glucose (mg/ dL) |
|
|
|
|
|
| ||||
Baseline | 250.5 | 247.5 | 253.9 | NS** | NS** | NS** | ||||
Change at FINAL VISIT | -63.5 | 13.7 | -0.9 | 0.001 | 0.001 | 0.025 | ||||
Hemoglobin A1c (%) |
|
|
|
|
|
| ||||
Baseline | 8.8 | 8.5 | 8.9 | NS** | NS** | 0.007 | ||||
Change at FINAL VISIT | -1.7 | 0.2 | -0.4 | 0.001 | 0.001 | 0.001 | ||||
Body Weight (lbs) |
|
|
|
|
|
| ||||
Baseline | 202.2 | 203.0 | 204.0 | NS** | NS** | NS** | ||||
Change at FINAL VISIT | 0.9 | -0.7 | -8.4 | 0.011 | 0.001 | 0.001 | ||||
The magnitude of the decline in fasting blood glucose concentration following the institution of metformin therapy was proportional to the level of fasting hyperglycemia. Patients with type 2 diabetes with higher fasting glucose concentrations experienced greater declines in plasma glucose and glycosylated hemoglobin.
In clinical studies, metformin, alone or in combination with a sulfonylurea, lowered mean fasting serum triglycerides, total cholesterol, and LDL cholesterol levels and had no adverse effects on other lipid levels (see Table 6).
Table 6. Summary of Mean Percent Change from Baseline of Major Serum Lipid Variables at Final Visit (29-week studies) | |||||
| Metformin vs Placebo | Combined Metformin/ Glyburide vs Monotherapy | |||
| Metformin (n = 141) | Placebo (n = 145) | Metformin (n = 210) | Metformin/ Glyburide (n = 213) | Glyburide (n = 209) |
Total Cholesterol (mg/dL) | |||||
Baseline | 211.0 | 212.3 | 213.1 | 215.6 | 219.6 |
Mean % Change at FINAL VISIT | -5% | 1% | -2% | -4% | 1% |
Total Triglycerides (mg/dL) | |||||
Baseline | 236.1 | 203.5 | 242.5 | 215.0 | 266.1 |
Mean % Change at FINAL VISIT | -16% | 1% | -3% | -8% | 4% |
LDL-Cholesterol (mg/dL) | |||||
Baseline | 135.4 | 138.5 | 134.3 | 136.0 | 137.5 |
Mean % Change at FINAL VISIT | -8% | 1% | -4% | -6% | 3% |
HDL-Cholesterol (mg/dL) | |||||
Baseline | 39.0 | 40.5 | 37.2 | 39.0 | 37.0 |
Mean % Change at FINAL VISIT | 2% | -1% | 5% | 3% | 1% |
In contrast to sulfonylureas, body weight of individuals on metformin tended to remain stable or even decrease somewhat (see Tables 4 and 5).
A 24-week, double-blind, placebo-controlled study of metformin plus insulin versus insulin plus placebo was conducted in patients with type 2 diabetes who failed to achieve adequate glycemic control on insulin alone (see Table 7). Patients randomized to receive metformin plus insulin achieved a reduction in HbA1c of 2.10%, compared to a 1.56% reduction in HbA1c achieved by insulin plus placebo. The improvement in glycemic control was achieved at the final study visit with 16% less insulin, 93.0 U/day vs. 110.6 U/day, metformin plus insulin versus insulin plus placebo, respectively, p = 0.04.
| a-Statistically significant using analysis of covariance with baseline as covariate (p = 0.04). Not significant using analysis of variance (values shown in table) | ||||||||||||||||||||
| b-Statistically significant for insulin (p = 0.04) | ||||||||||||||||||||
Table 7. Combined Metformin/Insulin vs Placebo/Insulin Summary of Mean Changes from Baseline in HbA1c and Daily Insulin Dose | ||||||||||||||||||||
| Metformin/Insulin (n = 26) | Placebo/Insulin (n = 28) | Treatment Difference Mean ± SE | |||||||||||||||||
Hemoglobin A1c (%) |
|
|
| |||||||||||||||||
Baseline | 8.95 | 9.32 | -0.54 ± 0.43a | |||||||||||||||||
Change at FINAL VISIT | -2.10 | -1.56 | ||||||||||||||||||
Insulin Dose (U/day) |
|
|
| |||||||||||||||||
Baseline | 93.12 | 94.64 | -16.08 ± 7.77b | |||||||||||||||||
Change at FINAL VISIT | -0.15 | 15.93 | ||||||||||||||||||
A second double-blind, placebo-controlled study (n = 51), with 16 weeks of randomized treatment, demonstrated that in patients with type 2 diabetes controlled on insulin for 8 weeks with an average HbA1c of 7.46 ± 0.97%, the addition of metformin maintained similar glycemic control (HbA1c 7.15 ± 0.61 versus 6.97 ± 0.62 for metformin plus insulin and placebo plus insulin, respectively) with 19% less insulin versus baseline (reduction of 23.68 ± 30.22 versus an increase of 0.43 ± 25.20 units for metformin plus insulin and placebo plus insulin, p < 0.01). In addition, this study demonstrated that the combination of metformin plus insulin resulted in reduction in body weight of 3.11 ± 4.30 lbs, compared to an increase of 1.30 ± 6.08 lbs for placebo plus insulin, p = 0.01.
Pediatric Clinical Studies
In a double-blind, placebo-controlled study in pediatric patients aged 10 to 16 years with type 2 diabetes (mean FPG 182.2 mg/dL), treatment with metformin (up to 2000 mg/day) for up to 16 weeks (mean duration of treatment 11 weeks) resulted in a significant mean net reduction in FPG of 64.3 mg/dL, compared with placebo (see Table 8).
| a-Pediatric patients mean age 13.8 years (range 10 - 16 years) | |||
| *- All patients on diet therapy at Baseline | |||
| **-Not statistically significant | |||
Table 8. Metformin vs Placebo (Pediatricsa) Summary of Mean Changes from Baseline* in Plasma Glucose and Body Weight at Final Visit | |||
| Metformin | Placebo | p-value |
FPG (mg/dL) | (n = 37) | (n = 36) | < 0.001 |
Baseline | 162.4 | 192.3 | |
Change at FINAL VISIT | -42.9 | 21.4 | |
Body Weight (lbs) | (n = 39) | (n = 38) | NS** |
Baseline | 205.3 | 189.0 | |
Change at FINAL VISIT | -3.3 | -2.0 | |
Indication And Usage
RIOMET (metformin hydrochloride oral solution) is indicated as an adjunct to diet and exercise to improve glycemic control in adults and children with type 2 diabetes mellitus.
Contraindications
RIOMET is contraindicated in patients with:
1. Severe renal impairment (eGFR below 30 mL/min/1.73 m2) (see WARNINGS and PRECAUTIONS).
2. Known hypersensitivity to metformin hydrochloride.
3. Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma. Diabetic ketoacidosis should be treated with insulin.
Warning: Lactic Acidosis
Post-marketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (> 5 mmol/Liter), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio; and metformin plasma levels generally > 5 mcg/mL [see Precautions].
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided [see Dosage and Administration, Contraindications, and Precautions].
If metformin-associated lactic acidosis is suspected, immediately discontinue RIOMET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended [see Precautions].
Precautions
General
Lactic Acidosis - There have been post-marketing cases of metformin-associated lactic acidosis, including fatal cases. These cases had a subtle onset and were accompanied by nonspecific symptoms such as malaise, myalgias, abdominal pain, respiratory distress, or increased somnolence; however, hypotension and resistant bradyarrhythmias have occurred with severe acidosis. Metformin-associated lactic acidosis was characterized by elevated blood lactate concentrations (> 5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), and an increases lactate:pyruvate ratio; metformin plasma levels were generally > 5 mcg/mL. Metformin decreases liver uptake of lactate increasing lactate blood levels which may increase the risk of lactic acidosis, especially in patients at risk.
If metformin-associated lactic acidosis is suspected, general supportive measures should be instituted promptly in a hospital setting, along with immediate discontinuation of RIOMET. In RIOMET treated patients with a diagnosis or strong suspicion of lactic acidosis, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin (metformin hydrochloride is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions). Hemodialysis has often resulted in reversal of symptoms and recovery.
Educate patients and their families about the symptoms of lactic acidosis and if these symptoms occur instruct them to discontinue RIOMET and report these symptoms to their healthcare provider.
For each of the known and possible risk factors for metformin-associated lactic acidosis, recommendations to reduce the risk of and manage metformin-associated lactic acidosis are provided below:
• Renal Impairment— The postmarketing metformin-associated lactic acidosis cases primarily occurred in patients with significant renal impairment. The risk of metformin accumulation and metformin-associated lactic acidosis increases with the severity of renal impairment because metformin is substantially excreted by the kidney. Clinical recommendations based upon the patient’s renal function include (see Dosage and Administration, Clinical Pharmacology):• Before initiating RIOMET, obtain an estimated glomerular filtration rate (eGFR).• RIOMET is contraindicated in patients with an eGFR less than 30 mL/min/1.73 m2 (see Contraindications).• Initiation of RIOMET is not recommended in patients with eGFR between 30-45 mL/min/1.73 m2.• Obtain an eGFR at least annually in all patients taking RIOMET. In patients at risk for the development of renal impairment (e.g., the elderly), renal function should be assessed more frequently.• In patients taking RIOMET whose eGFR falls below 45 mL/min/1.73 m2, assess the benefit and risk of continuing therapy.• Drug interactions—The concomitant use of RIOMET with specific drugs may increase the risk of metformin-associated lactic acidosis: those that impair renal function, result in significant hemodynamic change, interfere with acid-base balance, or increase metformin accumulation. Consider more frequent monitoring of patients.• Age 65 or Greater—The risk of metformin-associated lactic acidosis increases with the patient’s age because elderly patients have a greater likelihood of having hepatic, renal, or cardiac impairment than younger patients. Assess renal function more frequently in elderly patients.• Radiologic studies with contrast—Administration of intravascular iodinated contrast agents in metformin-treated patients has led to an acute decrease in renal function and the occurrence of lactic acidosis. Stop RIOMET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min/1.73 m2; in patients with a history of hepatic impairment, alcoholism or heart failure, or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure, and restart RIOMET if renal function is stable.• Surgery and other procedures—Withholding of food and fluids during surgical or other procedures may increase the risk for volume depletion, hypotension, and renal impairment. RIOMET should be temporarily discontinued while patients have restricted food and fluid intake.• Hypoxic states—Several of the postmarketing cases of metformin-associated lactic acidosis occurred in the setting of acute congestive heart failure (particularly when accompanied by hypoperfusion and hypoxemia). Cardiovascular collapse (shock), acute myocardial infarction, sepsis, and other conditions associated with hypoxemia have been associated with lactic acidosis and may cause prerenal azotemia. When such an event occurs, discontinue RIOMET.• Excessive Alcohol intake—Alcohol is known to potentiate the effect of metformin on lactate metabolism. Patients, therefore, should be warned against excessive alcohol intake, acute or chronic, while receiving RIOMET.• Hepatic impairment—Patients with hepatic impairment have developed cases of metformin-associated lactic acidosis. This may be due to impaired lactate clearance resulting in higher lactate blood levels. Therefore, avoid use of RIOMET in patients with clinical or laboratory evidence of hepatic disease.
Vitamin B12 levels — In controlled clinical trials of metformin of 29 weeks duration, a decrease to subnormal levels of previously normal serum Vitamin B12 levels, without clinical manifestations, was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, is, however, very rarely associated with anemia and appears to be rapidly reversible with discontinuation of metformin or Vitamin B12 supplementation. Measurement of hematologic parameters on an annual basis is advised in patients on RIOMET and any apparent abnormalities should be appropriately investigated and managed (see PRECAUTIONS: Laboratory Tests).
Certain individuals (those with inadequate Vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal Vitamin B12 levels. In these patients, routine serum Vitamin B12 measurements at two- to three-year intervals may be useful.
Hypoglycemia — Hypoglycemia does not occur in patients receiving metformin alone under usual circumstances of use, but could occur when caloric intake is deficient, when strenuous exercise is not compensated by caloric supplementation, or during concomitant use with other glucose-lowering agents (such as sulfonylureas and insulin) or ethanol.
Elderly, debilitated, or malnourished patients, and those with adrenal or pituitary insufficiency or alcohol intoxication are particularly susceptible to hypoglycemic effects. Hypoglycemia may be difficult to recognize in the elderly, and in people who are taking beta-adrenergic blocking drugs.
Macrovascular Outcomes
There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with RIOMET or any other oral anti-diabetic drug.
Information for Patients
Patients should be informed of the potential risks and benefits of RIOMET and of alternative modes of therapy. They should also be informed about the importance of adherence to dietary instructions, of a regular exercise program, and of regular testing of blood glucose, glycosylated hemoglobin, renal function, and hematologic parameters.
The risks of lactic acidosis, its symptoms, and conditions that predispose to its development, as noted in the WARNINGS and PRECAUTIONS sections, should be explained to patients. Patients should be advised to discontinue RIOMET immediately and to promptly notify their health practitioner if unexplained hyperventilation, myalgia, malaise, unusual somnolence, or other nonspecific symptoms occur. Once a patient is stabilized on any dose level of RIOMET, gastrointestinal symptoms, which are common during initiation of metformin therapy, are unlikely to be drug related. Later occurrence of gastrointestinal symptoms could be due to lactic acidosis or other serious disease.
Patients should be counseled against excessive alcohol intake, either acute or chronic, while receiving RIOMET.
Metformin alone does not usually cause hypoglycemia, although it may occur when metformin is used in conjunction with oral sulfonylureas and insulin. When initiating combination therapy, the risks of hypoglycemia, its symptoms and treatment, and conditions that predispose to its development should be explained to patients and responsible family members.
Laboratory Tests
Response to all diabetic therapies should be monitored by periodic measurements of fasting blood glucose and glycosylated hemoglobin levels, with a goal of decreasing these levels toward the normal range. During initial dose titration, fasting glucose can be used to determine the therapeutic response. Thereafter, both glucose and glycosylated hemoglobin should be monitored. Measurements of glycosylated hemoglobin may be especially useful for evaluating long-term control (see also DOSAGE AND ADMINISTRATION).
Initial and periodic monitoring of hematologic parameters (e.g., hemoglobin/hematocrit and red blood cell indices) and renal function (serum creatinine) should be performed, at least on an annual basis. While megaloblastic anemia has rarely been seen with metformin therapy, if this is suspected, Vitamin B12 deficiency should be excluded.
Instruct patients to inform their doctor that they are taking RIOMET prior to any surgical or radiological procedure, as temporary discontinuation of RIOMET may be required until renal function has been confirmed to be normal (see Precautions).
Drug Interactions (Clinical Evaluation of Drug Interactions Conducted with Metformin)
Glyburide — In a single-dose interaction study in type 2 diabetes patients, co-administration of metformin and glyburide did not result in any changes in either metformin pharmacokinetics or pharmacodynamics. Decreases in glyburide AUC and Cmax were observed, but were highly variable. The single-dose nature of this study and the lack of correlation between glyburide blood levels and pharmacodynamic effects, makes the clinical significance of this interaction uncertain (see DOSAGE AND ADMINISTRATION: Concomitant Metformin and Oral Sulfonylurea Therapy in Adult Patients).
Furosemide — A single-dose, metformin-furosemide drug interaction study in healthy subjects demonstrated that pharmacokinetic parameters of both compounds were affected by co-administration. Furosemide increased the metformin plasma and blood Cmax by 22% and blood AUC by 15%, without any significant change in metformin renal clearance. When administered with metformin, the Cmax and AUC of furosemide were 31% and 12% smaller, respectively, than when administered alone, and the terminal half-life was decreased by 32%, without any significant change in furosemide renal clearance. No information is available about the interaction of metformin and furosemide when co-administered chronically.
Nifedipine — A single-dose, metformin-nifedipine drug interaction study in normal healthy volunteers demonstrated that co-administration of nifedipine increased plasma metformin Cmax and AUC by 20% and 9%, respectively, and increased the amount excreted in the urine. Tmax and half-life were unaffected. Nifedipine appears to enhance the absorption of metformin. Metformin had minimal effects on nifedipine.
Drugs that reduce metformin clearance— Concomitant use of drugs that interfere with common renal tubular transport systems involved in the renal elimination of metformin (e.g., organic cationic transporter-2 [OCT2] / multidrug and toxin extrusion [MATE] inhibitors such as ranolazine, vandetanib, dolutegravir, and cimetidine) could increase systemic exposure to metformin and may increase the risk for lactic acidosis. Consider the benefits and risks of concomitant use. Such interaction between metformin and oral cimetidine has been observed in normal healthy volunteers in both single- and multiple-dose, metformin-cimetidine drug interaction studies, with a 60% increase in peak metformin plasma and whole blood concentrations and a 40% increase in plasma and whole blood metformin AUC. There was no change in elimination half-life in the single-dose study. Metformin had no effect on cimetidine pharmacokinetics.
In healthy volunteers, the pharmacokinetics of metformin and propranolol, and metformin and ibuprofen were not affected when co-administered in single-dose interaction studies.
Metformin is negligibly bound to plasma proteins and is, therefore, less likely to interact with highly protein-bound drugs such as salicylates, sulfonamides, chloramphenicol, and probenecid, as compared to the sulfonylureas, which are extensively bound to serum proteins.
Other — Certain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blocking drugs, and isoniazid. When such drugs are administered to a patient receiving RIOMET, the patient should be closely observed for loss of blood glucose control. When such drugs are withdrawn from a patient receiving RIOMET, the patient should be observed closely for hypoglycemia.
Carbonic Anhydrase Inhibitors --- Topiramate or other carbonic anhydrase inhibitors (e.g., zonisamide, acetazolamide or dichlorphenamide) frequently causes a decrease in serum bicarbonate and induce non-anion gap, hyperchloremic metabolic acidosis. Concomitant use of these drugs with RIOMET may increase the risk for lactic acidosis. Consider more frequent monitoring of these patients.
Alcohol --- Alcohol is known to potentiate the effect of metformin on lactate metabolism. Warn patients against excessive alcohol intake while receiving RIOMET.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies have been performed in rats (dosing duration of 104 weeks) and mice (dosing duration of 91 weeks), at doses up to and including 900 mg/kg/day and 1500 mg/kg/day, respectively.
These doses are both approximately four times the maximum recommended human daily dose of 2000 mg based on body surface area comparisons. No evidence of carcinogenicity with metformin was found in either male or female mice.
Similarly, there was no tumorigenic potential observed with metformin in male rats. There was, however, an increased incidence of benign stromal uterine polyps in female rats treated with 900 mg/kg/day.
There was no evidence of a mutagenic potential of metformin in the following in vitro tests: Ames test (S. typhimurium), gene mutation test (mouse lymphoma cells), or chromosomal aberrations test (human lymphocytes). Results in the in vivo mouse micronucleus test were also negative.
Fertility of male or female rats was unaffected by metformin when administered at doses as high as 600 mg/kg/day, which is approximately three times the maximum recommended human daily dose based on body surface area comparisons.
Pregnancy
Teratogenic Effects: Pregnancy Category B
Recent information strongly suggests that abnormal blood glucose levels during pregnancy are associated with a higher incidence of congenital abnormalities. Most experts recommend that insulin be used during pregnancy to maintain blood glucose levels as close to normal as possible. Because animal reproduction studies are not always predictive of human response, RIOMET should not be used during pregnancy unless clearly needed.
There are no adequate and well-controlled studies in pregnant women with metformin. Metformin was not teratogenic in rats and rabbits at doses up to 600 mg/kg/day. This represents an exposure of about two and six times the maximum recommended human daily dose of 2000 mg based on body surface area comparisons for rats and rabbits, respectively. Determination of fetal concentrations demonstrated a partial placental barrier to metformin.
Nursing Mothers
Studies in lactating rats show that metformin is excreted into milk and reaches levels comparable to those in plasma. Similar studies have not been conducted in nursing mothers. Because the potential for hypoglycemia in nursing infants may exist, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. If RIOMET is discontinued, and if diet alone is inadequate for controlling blood glucose, insulin therapy should be considered.
Pediatric Use
The safety and effectiveness of metformin for the treatment of type 2 diabetes have been established in pediatric patients ages 10 to 16 years (studies have not been conducted in pediatric patients below the age of 10 years). Use of metformin in this age group is supported by evidence from adequate and well-controlled studies of metformin in adults with additional data from a controlled clinical study in pediatric patients ages 10 to 16 years with type 2 diabetes, which demonstrated a similar response in glycemic control to that seen in adults. (See CLINICAL PHARMACOLOGY: Pediatric Clinical Studies.) In this study, adverse effects were similar to those described in adults. (See ADVERSE REACTIONS: Pediatric Patients.) A maximum daily dose of 2000 mg is recommended. (See DOSAGE AND ADMINISTRATION: Recommended Dosing Schedule: Pediatrics.)
Geriatric Use
Controlled clinical studies of metformin did not include sufficient numbers of elderly patients to determine whether they respond differently from younger patients, although other reported clinical experience has not identified differences in responses between the elderly and younger patients.
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy and the higher risk of lactic acidosis. Assess renal function more frequently in elderly patient (see also WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION).
Adverse Reactions
In a U.S. double-blind clinical study of metformin in patients with type 2 diabetes, a total of 141 patients received metformin therapy (up to 2550 mg per day) and 145 patients received placebo. Adverse reactions reported in greater than 5% of the metformin patients, and that were more common in metformin-than placebo-treated patients, are listed in Table 9.
| *-Reactions that were more common in metformin-than placebo-treated patients. | ||
Adverse Reaction | Metformin Monotherapy (n = 141) | Placebo (n = 145) |
% of patients | ||
Diarrhea | 53.2 | 11.7 |
Nausea/ Vomiting | 25.5 | 8.3 |
Flatulence | 12.1 | 5.5 |
Asthenia | 9.2 | 5.5 |
Indigestion | 7.1 | 4.1 |
Abdominal Discomfort | 6.4 | 4.8 |
Headache | 5.7 | 4.8 |
Diarrhea led to discontinuation of study medication in 6% of patients treated with metformin. Additionally, the following adverse reactions were reported in ≥ 1.0 to ≤ 5.0% of metformin patients and were more commonly reported with metformin than placebo: abnormal stools, hypoglycemia, myalgia, lightheaded, dyspnea, nail disorder, rash, sweating increased, taste disorder, chest discomfort, chills, flu syndrome, flushing, palpitation.
Pediatric Patients
In clinical trials with metformin in pediatric patients with type 2 diabetes, the profile of adverse reactions was similar to that observed in adults.
Cholestatic, hepatocellular, and mixed hepatocellular liver injury have been reported with postmarketing use of metformin.
Overdosage
Overdose of metformin hydrochloride has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no casual association with metformin hydrochloride has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases (see WARNINGS). Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
Dosage And Administration
There is no fixed dosage regimen for the management of hyperglycemia in patients with type 2 diabetes with RIOMET or any other pharmacologic agent. Dosage of RIOMET must be individualized on the basis of both effectiveness and tolerance, while not exceeding the maximum recommended daily doses. The maximum recommended daily dose of RIOMET is 2550 mg (25.5 mL) in adults and 2000 mg (20 mL) in pediatric patients (10 to 16 years of age).
RIOMET should be given in divided doses with meals. RIOMET should be started at a low dose, with gradual dose escalation, both to reduce gastrointestinal side effects and to permit identification of the minimum dose required for adequate glycemic control of the patient. During treatment initiation and dose titration (see Recommended Dosing Schedule), fasting plasma glucose should be used to determine the therapeutic response to RIOMET and identify the minimum effective dose for the patient. Thereafter, glycosylated hemoglobin should be measured at intervals of approximately three months. The therapeutic goal should be to decrease both fasting plasma glucose and glycosylated hemoglobin levels to normal or near normal by using the lowest effective dose of RIOMET, either when used as monotherapy or in combination with sulfonylurea or insulin.
Monitoring of blood glucose and glycosylated hemoglobin will also permit detection of primary failure, i.e., inadequate lowering of blood glucose at the maximum recommended dose of medication, and secondary failure, i.e., loss of an adequate blood glucose lowering response after an initial period of effectiveness.
Short-term administration of RIOMET may be sufficient during periods of transient loss of control in patients usually well-controlled on diet alone.
Recommendations For Use In Renal Impairment
Assess renal function prior to initiation of RIOMET and periodically thereafter.
RIOMET is contraindicated in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/minute/1.73 m2.
Initiation of RIOMET in patients with an eGFR between 30 – 45 mL/minute/1.73 m2 is not recommended.
In patients taking RIOMET whose eGFR later falls below 45 mL/min/1.73 m2, assess the benefit risk of continuing therapy.
Discontinue RIOMET if the patient’s eGFR later falls below 30 mL/minute/1.73 m2 (See WARNINGS and PRECAUTIONS).
Discontinuation For Iodinated Contrast Imaging Procedures
Discontinue RIOMET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/min/1.73 m2; in patients with a history of liver disease, alcoholism or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart RIOMET if renal function is stable.
Concomitant Metformin And Oral Sulfonylurea Therapy In Adult Patients
If patients have not responded to four weeks of the maximum dose of RIOMET monotherapy, consideration should be given to gradual addition of an oral sulfonylurea while continuing RIOMET at the maximum dose, even if prior primary or secondary failure to a sulfonylurea has occurred. Clinical and pharmacokinetic drug-drug interaction data are currently available only for metformin plus glyburide (glibenclamide).
With concomitant Metformin and sulfonylurea therapy, the desired control of blood glucose may be obtained by adjusting the dose of each drug. In a clinical trial of patients with type 2 diabetes and prior failure on glyburide, patients started on metformin 500 mg and glyburide 20 mg were titrated to 1000 mg/20 mg, 1500 mg/20 mg, 2000 mg/20 mg or 2500 mg/20 mg of metformin and glyburide, respectively, to reach the goal of glycemic control as measured by FPG, HbA1c and plasma glucose response (see CLINICAL PHARMACOLOGY: Clinical Studies). However, attempts should be made to identify the minimum effective dose of each drug to achieve this goal. With concomitant RIOMET and sulfonylurea therapy, the risk of hypoglycemia associated with sulfonylurea therapy continues and may be increased. Appropriate precautions should be taken. (See Package Insert of the respective sulfonylurea).
If patients have not satisfactorily responded to one to three months of concomitant therapy with the maximum dose of RIOMET and the maximum dose of an oral sulfonylurea, consider therapeutic alternatives including switching to insulin with or without RIOMET.
Concomitant Metformin And Insulin Therapy In Adult Patients
The current Insulin dose should be continued upon initiation of RIOMET therapy. RIOMET therapy should be initiated at 500 mg (5 mL) once daily in patients on insulin therapy. For patients not responding adequately, the dose of RIOMET should be increased by 500 mg (5 mL) after approximately 1 week and by 500 mg (5 mL) every week thereafter until adequate glycemic control is achieved. The maximum recommended daily dose for RIOMET is 2500 mg (25 mL). It is recommended that the insulin dose be decreased by 10% to 25% when fasting plasma glucose concentrations decrease to less than 120 mg/dL in patients receiving concomitant insulin and RIOMET. Further adjustment should be individualized based on glucose-lowering response.
Specific Patient Populations
RIOMET is not recommended for use in pregnancy. RIOMET is not recommended in patients below the age of 10 years.
The initial and maintenance dosing of RIOMET should be conservative in patients with advanced age, due to the potential for decreased renal function in this population. Any dosage adjustment should be based on a careful assessment of renal function.
Monitoring of renal function is necessary to aid in prevention of lactic acidosis, particularly in the elderly. (See WARNINGS.)
How Supplied
RIOMET (metformin hydrochloride oral solution) 500 mg/5 mL is a clear, colorless liquid with characteristic cherry or clear, colorless to light yellow liquid with characteristic strawberry flavor filled in 4 oz./16 oz. HDPE bottles with induction sealed child-resistant cap.
Cherry Flavor
NDC 10631-206-01 Bottles of 4 fl. oz. (118 mL)
NDC 10631-206-02 Bottles of 16 fl. oz. (473 mL)
Strawberry Flavor
STORAGE
Store at controlled room temperature 15° - 30° C (59° - 86° F) [See USP].
You may report side effects to FDA at 1-800-FDA-1088.
RIOMET is a registered trademark of Sun Pharmaceutical Industries Limited.
Manufactured for:
Ranbaxy Laboratories Inc.
Jacksonville, FL 32257 USA
Package/Label Display Panel
10631-206-01
RIOMET®(metformin hydrochloride oral solution)
500 mg/5 mL
Each 5 mL contains: 500 mg of metformin hydrochloride, USP.
Cherry Flavor
Rx only
4 fl. Oz. 118 mL
NDC 10631-238-01
RIOMET®(metformin hydrochloride oral solution)
500 mg/5 mL E
ach 5 mL contains: 500 mg of metformin hydrochloride, USP.
Strawberry Flavor
Rx only 4 fl. Oz. 118 mL
* Please review the disclaimer below.