FDA Label for Rivastigmine Transdermal System
View Indications, Usage & Precautions
- 1 INDICATIONS AND USAGE
- 1.1 ALZHEIMER’S DISEASE
- 1.2 PARKINSON’S DISEASE DEMENTIA
- 2 DOSAGE AND ADMINISTRATION
- 2.1 RECOMMENDED DOSING
- 2.2 DOSING IN SPECIFIC POPULATIONS
- 2.3 SWITCHING TO RIVASTIGMINE PATCH FROM RIVASTIGMINE CAPSULES OR RIVASTIGMINE ORAL SOLUTION
- 2.4 IMPORTANT ADMINISTRATION INSTRUCTIONS
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 MEDICATION ERRORS RESULTING IN OVERDOSE
- 5.2 GASTROINTESTINAL ADVERSE REACTIONS
- 5.3 SKIN REACTIONS
- 5.4 OTHER ADVERSE REACTIONS FROM INCREASED CHOLINERGIC ACTIVITY
- 5.5 IMPAIRMENT IN DRIVING OR USE OF MACHINERY
- 5.6 MRI SKIN BURNS
- 6 ADVERSE REACTIONS
- 6.1 CLINICAL TRIALS EXPERIENCE
- 6.2 POSTMARKETING EXPERIENCE
- 7 DRUG INTERACTIONS
- 7.1 METOCLOPRAMIDE
- 7.2 CHOLINOMIMETIC AND ANTICHOLINERGIC MEDICATIONS
- 7.3 BETA-BLOCKERS
- 8 USE IN SPECIFIC POPULATIONS
- 8.1 PREGNANCY
- 8.3 NURSING MOTHERS
- 8.4 PEDIATRIC USE
- 8.5 GERIATRIC USE
- 8.6 HEPATIC IMPAIRMENT
- 8.7 LOW OR HIGH BODY WEIGHT
- 10 OVERDOSAGE
- 11 DESCRIPTION
- 12.1 MECHANISM OF ACTION
- 12.2 PHARMACODYNAMICS
- 12.3 PHARMACOKINETICS
- 13 NONCLINICAL TOXICOLOGY
- 13.1 CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- PATIENT INFORMATION
- INSTRUCTIONS FOR USE
- CARTON - 4.6 MG/24 HOURS
- POUCH - 4.6 MG/24 HOURS
- CARTON - 9.5 MG/24 HOURS
- POUCH - 9.5 MG/24 HOURS
- CARTON - 13.3 MG/24 HOURS
- POUCH - 13.3 MG/24 HOURS
Rivastigmine Transdermal System Product Label
The following document was submitted to the FDA by the labeler of this product Alvogen Inc.. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
1 Indications And Usage
1.1 Alzheimer’S Disease
Rivastigmine Patch is indicated for the treatment of dementia of the Alzheimer’s type (AD). Efficacy has been demonstrated in patients with mild to moderate Alzheimer’s disease.
1.2 Parkinson’S Disease Dementia
Rivastigmine Patch is indicated for the treatment of mild to moderate dementia associated with Parkinson’s disease (PDD).
2 Dosage And Administration
2.1 Recommended Dosing
Initial Dose
Initiate treatment with one 4.6 mg/24 hours Rivastigmine Patch applied to the skin once daily [see Dosage and Administration (2.4)].
Dose Titration
Increase the dose only after a minimum of 4 weeks at the previous dose, and only if the previous dose has been tolerated. For mild to moderate AD and PDD patients, continue the effective dose of 9.5 mg/24 hours for as long as therapeutic benefit persists. Patients can then be increased to the maximum effective dose of 13.3 mg/24 hours dose. Doses higher than 13.3 mg/24 hours confer no appreciable additional benefit, and are associated with an increase in the incidence of adverse reactions [see Warnings and Precautions (5.2), Adverse Reactions (6.1)].
Mild to Moderate Alzheimer’s Disease and Mild to Moderate Parkinson’s Disease Dementia
The effective dosage of Rivastigmine Patch is 9.5 mg/24 hours or 13.3 mg/24 hours administered once per day; replace with a new patch every 24 hours.
Interruption of Treatment
If dosing is interrupted for 3 days or fewer, restart treatment with the same or lower strength Rivastigmine Patch. If dosing is interrupted for more than 3 days, restart treatment with the 4.6 mg/24 hours Rivastigmine Patch and titrate as described above.
2.2 Dosing In Specific Populations
Dosing Modifications in Patients with Hepatic Impairment
Consider using the 4.6 mg/24 hours Rivastigmine Patch as both the initial and maintenance dose in patients with mild (Child-Pugh score 5 to 6) to moderate (Child-Pugh score 7 to 9) hepatic impairment [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
Dosing Modifications in Patients with Low Body Weight
Carefully titrate and monitor patients with low body weight (<50 kg) for toxicities (e.g., excessive nausea, vomiting) and consider reducing the maintenance dose to the 4.6 mg/24 hours Rivastigmine Patch if such toxicities develop.
2.3 Switching To Rivastigmine Patch From Rivastigmine Capsules Or Rivastigmine Oral Solution
Patients treated with rivastigmine capsules or oral solution may be switched to Rivastigmine Patch as follows:
- A patient who is on a total daily dose of <6 mg of oral rivastigmine can be switched to the 4.6 mg/24 hours Rivastigmine Patch.
- A patient who is on a total daily dose of 6 mg to 12 mg of oral rivastigmine can be switched to the 9.5 mg/24 hours Rivastigmine Patch.
Instruct patients or caregivers to apply the first patch on the day following the last oral dose.
2.4 Important Administration Instructions
Rivastigmine Patch is for transdermal use on intact skin.
(a) Do not use the patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way.
(b) Apply the Rivastigmine Patch once a day
- Press down firmly for 30 seconds until the edges stick well when applying to clean, dry, hairless, intact healthy skin in a place that will not be rubbed against by tight clothing.
- Use the upper or lower back as the site of application because the patch is less likely to be removed by the patient. If sites on the back are not accessible, apply the patch to the upper arm or chest.
- Do not apply to a skin area where cream, lotion, or powder has recently been applied.
(c) Do not apply to skin that is red, irritated, or cut.
(d) Replace the Rivastigmine Patch with a new patch every 24 hours. Instruct patients to only wear one patch at a time (remove the previous day's patch before applying a new patch) [see Warnings and Precautions (5.1) and Overdosage (10)]. If a patch falls off or if a dose is missed, apply a new patch immediately and then replace this patch the following day at the usual application time.
(e) Change the site of patch application daily to minimize potential irritation, although a new patch can be applied to the same general anatomic site (e.g., another spot on the upper back) on consecutive days. Do not apply a new patch to the same location for at least 14 days.
(f) May wear the patch during bathing and in hot weather. But avoid long exposure to external heat sources (excessive sunlight, saunas, solariums).
(g) Place used patches in the previously saved pouch and discard in the trash, away from pets or children.
(h) Wash hands with soap and water after removing the patch. In case of contact with eyes or if the eyes become red after handling the patch, rinse immediately with plenty of water and seek medical advice if symptoms do not resolve.
3 Dosage Forms And Strengths
Rivastigmine Patch is available in 3 strengths. Each patch has a tan backing layer labeled as either:
- Rivastigmine Patch 4.6 mg/24 hours, “RIVASTIGMINE 4.6 mg/24 hr”
- Rivastigmine Patch 9.5 mg/24 hours, “RIVASTIGMINE 9.5 mg/24 hr”
- Rivastigmine Patch 13.3 mg/24 hours, "RIVASTIGMINE 13.3 mg/24 hr"
4 Contraindications
Rivastigmine Patch is contraindicated in patients with:
- known hypersensitivity to rivastigmine, other carbamate derivatives, or other components of the formulation [see Description (11)].
- previous history of application site reactions with rivastigmine transdermal patch suggestive of allergic contact dermatitis [see Warnings and Precautions (5.3)].
Isolated cases of generalized skin reactions have been described in postmarketing experience [see Adverse Reactions (6.2)].
5 Warnings And Precautions
5.1 Medication Errors Resulting In Overdose
Medication errors with Rivastigmine Patch have resulted in serious adverse reactions; some cases have required hospitalization, and rarely, led to death. The majority of medication errors have involved not removing the old patch when putting on a new one and the use of multiple patches at one time.
Instruct patients and their caregivers on important administration instructions for Rivastigmine Patch [see Dosage and Administration (2.4)].
5.2 Gastrointestinal Adverse Reactions
Rivastigmine Patch can cause gastrointestinal adverse reactions, including significant nausea, vomiting, diarrhea, anorexia/decreased appetite, and weight loss. Dehydration may result from prolonged vomiting or diarrhea and can be associated with serious outcomes. The incidence and severity of these reactions are dose-related [see Adverse Reactions (6.1)]. For this reason, initiate treatment with Rivastigmine Patch at a dose of 4.6 mg/24 hours and titrate to a dose of 9.5 mg/24 hours and then to a dose of 13.3 mg/24 hours, if appropriate [see Dosage and Administration (2.1)].
If treatment is interrupted for more than 3 days because of intolerance, reinitiate Rivastigmine Patch with the 4.6 mg/24 hours dose to reduce the possibility of severe vomiting and its potentially serious sequelae. A postmarketing report described a case of severe vomiting with esophageal rupture following inappropriate reinitiation of treatment of an oral formulation of rivastigmine without retitration after 8 weeks of treatment interruption.
Inform caregivers to monitor for gastrointestinal adverse reactions and to inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than 3 days because of intolerance, the next dose should not be administered without contacting the physician regarding proper retitration.
5.3 Skin Reactions
Skin application site reactions may occur with Rivastigmine Patch. These reactions are not in themselves an indication of sensitization. However, use of rivastigmine patch may lead to allergic contact dermatitis.
Allergic contact dermatitis should be suspected if application site reactions spread beyond the patch size, if there is evidence of a more intense local reaction (e.g. increasing erythema, edema, papules, vesicles) and if symptoms do not significantly improve within 48 hours after patch removal. In these cases, treatment should be discontinued [see Contraindications (4)].
In patients who develop application site reactions to Rivastigmine Patch suggestive of allergic contact dermatitis and who still require rivastigmine, treatment should be switched to oral rivastigmine only after negative allergy testing and under close medical supervision. It is possible that some patients sensitized to rivastigmine by exposure to rivastigmine patch may not be able to take rivastigmine in any form.
There have been isolated postmarketing reports of patients experiencing disseminated allergic dermatitis when administered rivastigmine irrespective of the route of administration (oral or transdermal). In these cases, treatment should be discontinued [see Contraindications (4)]. Patients and caregivers should be instructed accordingly.
5.4 Other Adverse Reactions From Increased Cholinergic Activity
Neurologic Effects
Extrapyramidal Symptoms: Cholinomimetics, including rivastigmine, may exacerbate or induce extrapyramidal symptoms. Worsening of parkinsonian symptoms, particularly tremor, has been observed in patients with dementia associated with Parkinson’s disease who were treated with rivastigmine capsules.
Seizures: Drugs that increase cholinergic activity are believed to have some potential for causing seizures. However, seizure activity also may be a manifestation of Alzheimer's disease.
Peptic Ulcers/Gastrointestinal Bleeding
Cholinesterase inhibitors, including rivastigmine, may increase gastric acid secretion due to increased cholinergic activity. Monitor patients using Rivastigmine Patch for symptoms of active or occult gastrointestinal bleeding, especially those at increased risk for developing ulcers, e.g., those with a history of ulcer disease or those receiving concurrent nonsteroidal anti-inflammatory drugs (NSAIDs). Clinical studies of rivastigmine have shown no significant increase, relative to placebo, in the incidence of either peptic ulcer disease or gastrointestinal bleeding.
Use with Anesthesia
Rivastigmine, as a cholinesterase inhibitor, is likely to exaggerate succinylcholine-type muscle relaxation during anesthesia.
Cardiac Conduction Effects
Because rivastigmine increases cholinergic activity, use of the Rivastigmine Patch may have vagotonic effects on heart rate (e.g., bradycardia). The potential for this action may be particularly important in patients with sick sinus syndrome or other supraventricular cardiac conduction conditions. In clinical trials, rivastigmine was not associated with any increased incidence of cardiovascular adverse events, heart rate or blood pressure changes, or ECG abnormalities.
Genitourinary Effects
Although not observed in clinical trials of rivastigmine, drugs that increase cholinergic activity may cause urinary obstruction.
Pulmonary Effects
Drugs that increase cholinergic activity, including Rivastigmine Patch should be used with care in patients with a history of asthma or obstructive pulmonary disease.
5.5 Impairment In Driving Or Use Of Machinery
Dementia may cause gradual impairment of driving performance or compromise the ability to use machinery. The administration of rivastigmine may also result in adverse reactions that are detrimental to these functions. During treatment with Rivastigmine Patch, routinely evaluate the patient's ability to continue driving or operating machinery.
5.6 Mri Skin Burns
Skin burns have been reported at the patch site in several patients wearing an aluminized transdermal system during a Magnetic Resonance Imaging scan (MRI). Because the Rivastigmine Patch contains aluminum, it is recommended to remove the system before undergoing an MRI.
6 Adverse Reactions
The following adverse reactions are described below and elsewhere in the labeling:
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Rivastigmine Patch has been administered to 4516 patients with Alzheimer's disease during clinical trials worldwide. Of these, 3005 patients have been treated for at least 26 weeks, 1771 patients have been treated for at least 52 weeks, 974 patients have been treated for at least 78 weeks and 24 patients have been treated for at least 104 weeks.
Mild to Moderate Alzheimer’s Disease
24-Week International Placebo-Controlled Trial (Study 1)
Most Common Adverse Reactions
The most common adverse reactions in patients administered Rivastigmine Patch in Study 1 [see Clinical Studies (14)], defined as those occurring at a frequency of at least 5% in the 9.5 mg/24 hours Rivastigmine Patch arm and at a frequency at higher than in the placebo group, were nausea, vomiting, and diarrhea. These reactions were dose-related, with each being more common in patients using the unapproved 17.4 mg/24 hours Rivastigmine Patch than in those using the 9.5 mg/24 hours Rivastigmine Patch.
Discontinuation Rates
In Study 1, which randomized a total of 1195 patients, the proportions of patients in the Rivastigmine Patch 9.5 mg/24 hours, rivastigmine capsules 6 mg twice daily, and placebo groups who discontinued treatment due to adverse events were 10%, 8%, and 5%, respectively.
The most common adverse reactions in the Rivastigmine Patch-treated groups that led to treatment discontinuation in this study were nausea and vomiting. The proportions of patients who discontinued treatment due to nausea were 0.7%, 1.7%, and 1.3% in the Rivastigmine Patch 9.5 mg/24 hours, rivastigmine capsules 6 mg twice daily, and placebo groups, respectively. The proportions of patients who discontinued treatment due to vomiting were 0%, 2.0%, and 0.3% in the Rivastigmine Patch 9.5 mg/24 hours, rivastigmine capsules 6 mg twice daily, and placebo groups, respectively.
Adverse Reactions Observed at an Incidence of ≥2%
Table 1 lists adverse reactions seen at an incidence of ≥2% in either Rivastigmine Patch-treated group in Study 1 and for which the rate of occurrence was greater for patients treated with that dose of Rivastigmine Patch than for those treated with placebo. The unapproved 17.4 mg/24 hours Rivastigmine Patch arm is included to demonstrate the increased rates of gastrointestinal adverse reactions over those seen with the 9.5 mg/24 hours Rivastigmine Patch.
Table 1: Proportion of Adverse Reactions Observed with a Frequency of ≥2% and Occurring at a Rate Greater Than Placebo in Study 1
| Rivastigmine Patch 9.5 mg/24 hours | Rivastigmine Patch 17.4 mg/24hours | Rivastigmine capsule 6 mg twice daily | Placebo | |
| Total Patients Studied | 291 | 303 | 294 | 302 |
| Total Percentage of Patients with ARs (%) | 51 | 66 | 63 | 46 |
| Nausea | 7 | 21 | 23 | 5 |
| Vomiting Vomiting was severe in 0% of patients who received Rivastigmine Patch 9.5 mg/24 hours, 1% of patients who received Rivastigmine Patch 17.4 mg/24 hours, 1% of patients who received the rivastigmine capsule at doses up to 6 mg twice daily, and 0% of those who received placebo. | 6 | 19 | 17 | 3 |
| Diarrhea | 6 | 10 | 5 | 3 |
| Depression | 4 | 4 | 4 | 1 |
| Headache | 3 | 4 | 6 | 2 |
| Anxiety | 3 | 3 | 2 | 1 |
| Anorexia/Decreased Appetite | 3 | 9 | 9 | 2 |
| Weight Decreased Weight Decreased as presented in Table 1 is based upon clinical observations and/or adverse events reported by patients or caregivers. Body weight was also monitored at prespecified time points throughout the course of the clinical study. The proportion of patients who had weight loss equal to or greater than 7% of their baseline weight was 8% of those treated with Rivastigmine Patch 9.5 mg/24 hours, 12% of those treated with Rivastigmine Patch 17.4 mg/24 hours, 11% of patients who received the rivastigmine capsule at doses up to 6 mg twice daily and 6% of those who received placebo. It is not clear how much of the weight loss was associated with anorexia, nausea, vomiting, and the diarrhea associated with the drug. | 3 | 8 | 5 | 1 |
| Dizziness | 2 | 7 | 7 | 2 |
| Abdominal Pain | 2 | 4 | 1 | 1 |
| Urinary Tract Infection | 2 | 2 | 1 | 1 |
| Asthenia | 2 | 3 | 6 | 1 |
| Fatigue | 2 | 2 | 1 | 1 |
| Insomnia | 1 | 4 | 2 | 2 |
| Abdominal Pain Upper | 1 | 3 | 2 | 2 |
| Vertigo | 0 | 2 | 1 | 1 |
48-Week International Active Comparator-Controlled Trial (Study 2)
Most Common Adverse Reactions
In Study 2 [see Clinical Studies (14)] of the commonly observed adverse reactions (≥3% in any treatment group) the most frequent events in the Rivastigmine Patch 13.3 mg/24 hours group were nausea, followed by vomiting, fall, weight decreased, application site erythema, decreased appetite, diarrhea and urinary tract infection (Table 3). The percentage of patients with these events was higher in the Rivastigmine Patch 13.3 mg/24 hours group than in the Rivastigmine Patch 9.5 mg/24 hours group. Patients with nausea, vomiting, diarrhea and decreased appetite experienced these reactions more often during the first 4 weeks of the double-blind treatment phase. These reactions decreased over time in each treatment group. Weight decreased was reported to have increased over time in each treatment group.
Discontinuation Rates
Table 2 displays the most common adverse reactions leading to discontinuation during the 48-week, double-blind treatment phase in Study 2.
Table 2: Proportion of Most Common Adverse Reactions (>1% at Any Dose) Leading to Discontinuation During 48-week Double-Blind Treatment Phase in Study 2
| Rivastigmine Patch 13.3 mg/24 hours | Rivastigmine Patch 9.5 mg/24 hours | Total | |
| Total Patients Studied | 280 | 283 | 563 |
| Total Percentage of Patients with ARs Leading to Discontinuation (%) | 9.6 | 12.7 | 11.2 |
| Vomiting | 1.4 | 0.4 | 0.9 |
| Application site pruritus | 1.1 | 1.1 | 1.1 |
| Aggression | 0.4 | 1.1 | 0.7 |
Most Common Adverse Reactions ≥3%
Other adverse reactions of interest which occurred less frequently, but which were observed in a markedly higher percentage of patients in the Rivastigmine Patch 13.3 mg/24 hours group than in the Rivastigmine Patch 9.5 mg/24 hours group in Study 2, included dizziness and upper abdominal pain. The percentage of patients with these reactions decreased over time in each treatment group (Table 3). The adverse reaction severity profile was generally similar for both the Rivastigmine Patch 13.3 mg/24 hours and 9.5 mg/24 hours groups.
Table 3: Proportion of Adverse Reactions Over Time in the 48-week Double-Blind (DB) Treatment Phase (at Least 3% in any Treatment Group) in Study 2
| Cumulative Week 0 to 48 (DB Phase) | Week 0 to 24 (DB Phase) | Week >24 to 48 (DB Phase) | ||||
| Preferred Term | Rivastigmine Patch 13.3 mg/24 hours | Rivastigmine Patch 9.5 mg/24 hours | Rivastigmine Patch 13.3 mg/24 hours | Rivastigmine Patch 9.5 mg/24 hours | Rivastigmine Patch 13.3 mg/24 hours | Rivastigmine Patch 9.5 mg/24 hours |
| Total Patients Studied | 280 | 283 | 280 | 283 | 241 | 246 |
| Total Percentage of Patients with ARs (%) | 75 | 68 | 65 | 55 | 42 | 40 |
| Nausea | 12 | 5 | 10 | 4 | 4 | 2 |
| Vomiting | 10 | 5 | 9 | 3 | 3 | 2 |
| Fall | 8 | 6 | 4 | 4 | 4 | 3 |
| Weight decreased Decreased Weight as presented in Table 3 is based upon clinical observations and/or adverse events reported by patients or caregivers. Body weight was monitored as a vital sign at pre-specified time points throughout the course of the clinical study. The proportion of patients who had weight loss equal to or greater than 7% of their baseline weight was 15.2% of those treated with Rivastigmine Patch 9.5 mg/24 hours and 18.6% of those treated with Rivastigmine Patch 13.3 mg/24 hours during the 48 week double-blind treatment period | 7 | 3 | 3 | 1 | 5 | 2 |
| Application site erythema | 6 | 6 | 6 | 5 | 1 | 2 |
| Decreased appetite | 6 | 3 | 5 | 2 | 2 | <1 |
| Diarrhea | 6 | 5 | 5 | 4 | 2 | <1 |
| Urinary tract infection | 5 | 4 | 3 | 3 | 3 | 2 |
| Agitation | 5 | 5 | 4 | 3 | 1 | 2 |
| Depression | 5 | 5 | 3 | 3 | 3 | 2 |
| Dizziness | 4 | 1 | 3 | <1 | 2 | <1 |
| Application site pruritus | 4 | 4 | 4 | 3 | <1 | 1 |
| Headache | 4 | 4 | 4 | 4 | <1 | <1 |
| Insomnia | 4 | 3 | 2 | 1 | 3 | 2 |
| Abdominal pain upper | 4 | 1 | 3 | 1 | 1 | <1 |
| Anxiety | 4 | 3 | 2 | 2 | 2 | 1 |
| Hypertension | 3 | 3 | 3 | 2 | 1 | 1 |
| Urinary incontinence | 3 | 2 | 2 | 1 | 1 | <1 |
| Psychomotor hyperactivity | 3 | 3 | 2 | 3 | 2 | 1 |
| Aggression | 2 | 3 | 1 | 3 | 1 | 1 |
24-Week US Controlled Trial
Most Commonly Observed Adverse Reactions
The most common adverse reactions in patients administered Rivastigmine Patch in the controlled clinical trial, defined as those occurring at a frequency of at least 5% in the 13.3 mg/24 hours Rivastigmine Patch arm and at a frequency higher than in the 4.6 mg/24 hours Rivastigmine Patch were application site erythema, fall, insomnia, vomiting, diarrhea, weight decreased, and nausea (Table 4). Patients in the lower dose group reported more events of agitation, urinary tract infection, and hallucinations than patients in the higher dose group.
Discontinuation Rates
The proportions of patients in the Rivastigmine Patch 13.3 mg/24 hours (n=355) and Rivastigmine Patch 4.6 mg/24 hours (n=359), who discontinued treatment due to adverse reactions were 21% and 14%, respectively.
The most frequent adverse reaction leading to discontinuation in the 13.3 mg/24 hours treatment group versus the 4.6 mg/24 hours treatment group was agitation (2.8% versus 2.2%), followed by vomiting (2.5% and 1.1%), nausea (1.7% and 1.1%), decreased appetite (1.7% and 0%), aggression (1.1% and 0.3%), fall (1.1% and 0.3%) and syncope (1.1% and 0.3%). Otherwise, all AEs leading to discontinuation were reported in <1% of patients.
Most Commonly Observed Adverse Reactions ≥5%
Other adverse reactions of interest which were observed in a higher percentage of patients in the Rivastigmine Patch 13.3 mg/24 hours group than in the Rivastigmine Patch 4.6 mg/24 hours group, included application site erythema, fall, insomnia, vomiting, diarrhea, weight decreased, and nausea (Table 4). Overall, the majority of patients in this study experienced adverse reactions that were mild (30.7%) or moderate (32.1%) in severity. Slightly more patients in the 4.6 mg/24 hours patch group reported mild events than in the 13.3 mg/24 hours patch group, while the numbers of patients reporting moderate events were comparable between groups. Severe adverse reactions were reported at a slightly higher percentage at the higher dose (12.4%) than at the lower dose (10%) treatment groups. With the exception of severe adverse reactions of agitation (13.3 mg: 1.1%; 4.6 mg: 1.4%), fall (13.3 mg: 1.1%) and urinary tract infection (4.6 mg: 1.1%), all adverse reactions reported as severe occurred in less than 1% of patients in either treatment group.
Table 4: Proportion of Adverse Reactions in the 24-week Double Blind (DB) Treatment Phase (at Least 5% in Any Treatment group)
| Preferred term | Rivastigmine Patch | Rivastigmine Patch |
| 13.3 mg/24 hours | 4.6 mg/24 hours | |
| Total number of patients studied | 355 | 359 |
| Total percentage of patients with ARs (%) | 75 | 73 |
| Application site erythema | 13 | 12 |
| Agitation | 12 | 14 |
| Urinary tract infection | 8 | 10 |
| Fall | 8 | 6 |
| Insomnia | 7 | 4 |
| Vomiting | 7 | 3 |
| Diarrhea | 7 | 5 |
| Weight decreased Weight Decreased as presented in Table 4 is based upon clinical observations and/or adverse events reported by patients or caregivers. Body weight was monitored as a vital sign at prespecified time points throughout the course of the clinical study. The proportion of patients who had weight loss equal to or greater than 7% of their baseline weight was 11% of those treated with Rivastigmine Patch 4.6 mg/24 hours and 14.1% of those treated with Rivastigmine Patch 13.3 mg/24 hours during the 24-week double-blind treatment. | 7 | 3 |
| Nausea | 6 | 3 |
| Depression | 5 | 4 |
| Decreased appetite | 5 | 1 |
| Anxiety | 5 | 5 |
| Hallucination | 2 | 5 |
Application Site Reactions
Application site skin reactions leading to discontinuation were observed in ≤2.3% of Rivastigmine Patch patients. This number was 4.9% and 8.4% in the Chinese population and Japanese population, respectively.
Cases of skin irritation were captured separately on an investigator-rated skin irritation scale. Skin irritation, when observed, was mostly slight or mild in severity and was rated as severe in ≤2.2% of Rivastigmine Patch patients in a double-blind controlled study and in ≤3.7% of Rivastigmine Patch patients in a double-blind controlled study in Japanese patients.
Parkinson’s Disease Dementia
76-week International Open Label Trial (Study 4)
Rivastigmine Patch has been administered to 288 patients with mild to moderate Parkinson’s Disease Dementia in a single, 76-week, open-label, active-comparator safety study. Of these, 256 have been treated for at least 12 weeks, 232 for at least 24 weeks, and 196 for at least 52 weeks.
Treatment with Rivastigmine patch was initiated at 4.6 mg/24 hours and if tolerated the dose was increased after 4 weeks to 9.5 mg/24 hours. Rivastigmine capsule (target maintenance dose of 12 mg/day) served as the active comparator and was administered to 294 patients. Adverse reactions are presented in Table 5.
Table 5: Proportion of Adverse Reactions Reported at a Rate ≥2% During the Initial 24-Week Period in Study 4
| Adverse drug reactions | Rivastigmine Patch |
| Total patients studied | 288 |
| Percentage (%) | |
| Psychiatric disorders | |
| Insomnia | 6 |
| Depression | 6 |
| Anxiety | 5 |
| Agitation | 3 |
| Nervous system disorders | |
| Tremor | 7 |
| Dizziness | 6 |
| Somnolence | 4 |
| Hypokinesia | 4 |
| Bradykinesia | 4 |
| Cogwheel rigidity | 3 |
| Dyskinesia | 3 |
| Gastrointestinal disorders Abdominal pain | 2 |
| Vascular disorders Hypertension | 3 |
| General disorders and administration site conditions | |
| Fall | 12 |
| Application site erythema | 11 |
| Application site irritation, pruritus, rash | 3; 5; 2 |
| Fatigue | 4 |
| Asthenia | 2 |
| Gait disturbance | 4 |
Additional adverse reactions observed during the 76-week prospective, open-label study in patients with dementia associated with Parkinson’s disease treated with Rivastigmine patches: Frequent (those occurring in at least 1/100 patients): dehydration, weight decreased, aggression, hallucination visual.
In patients with dementia associated with Parkinson’s disease the following adverse drug reactions have only been observed in clinical trials with rivastigmine capsules: Frequent: nausea, vomiting, decreased appetite, restlessness, worsening of Parkinson’s disease, bradycardia, diarrhea, dyspepsia, salivary hypersecretion, sweating increased; Infrequent (those occurring between 1/100 to 1/1000 patients): dystonia, atrial fibrillation, atrioventricular block.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of rivastigmine capsules, rivastigmine oral solution or Rivastigmine Patch. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac Disorders: Tachycardia.
Hepatobiliary Disorders: Abnormal liver function tests, hepatitis.
Nervous System Disorders: Parkinson’s disease (worsening), seizure, tremor.
Psychiatric Disorders: nightmares.
Skin and Subcutaneous Tissue Disorders: Allergic dermatitis, application site hypersensitivity, blister, disseminated allergic dermatitis, Stevens-Johnson syndrome, urticaria.
Vascular Disorders: Hypertension.
7 Drug Interactions
7.1 Metoclopramide
Due to the risk of additive extra-pyramidal adverse reactions, the concomitant use of metoclopramide and Rivastigmine Patch is not recommended.
7.2 Cholinomimetic And Anticholinergic Medications
Rivastigmine Patch may increase the cholinergic effects of other cholinomimetic medications and may also interfere with the activity of anticholinergic medications (e.g., oxybutynin, tolterodine). Concomitant use of Rivastigmine Patch with medications having these pharmacologic effects is not recommended unless deemed clinically necessary [see Warnings and Precautions (5.4)].
7.3 Beta-Blockers
Additive bradycardic effects resulting in syncope may occur when rivastigmine is used concomitantly with beta-blockers, especially cardioselective beta-blockers (including atenolol). Concomitant use is not recommended when signs of bradycardia including syncope are present.
8 Use In Specific Populations
8.1 Pregnancy
Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. No dermal reproduction studies in animals have been conducted.
Oral reproduction studies conducted in pregnant rats and rabbits revealed no evidence of teratogenicity. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Rivastigmine and its metabolites are excreted in rat milk following oral administration of rivastigmine; levels of rivastigmine plus metabolites in rat milk are approximately 2 times that in maternal plasma. It is not known whether rivastigmine is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Rivastigmine Patch, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Use of Rivastigmine Patch in pediatric patients (below 18 years of age) is not recommended.
8.5 Geriatric Use
Of the total number of patients in clinical studies of Rivastigmine Patch, 88% were 65 years and over, while 55% were 75 years. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
Increased exposure to rivastigmine was observed in patients with mild or moderate hepatic impairment with oral rivastigmine. Patients with mild or moderate hepatic impairment may be able to only tolerate lower doses [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)]. No data are available on the use of rivastigmine in patients with severe hepatic impairment.
8.7 Low Or High Body Weight
Because rivastigmine blood levels vary with weight, careful titration and monitoring should be performed in patients with low or high body weights [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
10 Overdosage
Overdose with Rivastigmine Patch has been reported in the postmarketing setting [see Warnings and Precautions (5.1)]. Overdoses have occurred from application of more than one patch at one time and not removing the previous day’s patch before applying a new patch. The symptoms reported in these overdose cases are similar to those seen in cases of overdose associated with rivastigmine oral formulations.
Because strategies for the management of overdose are continually evolving, it is advisable to contact a Poison Control Center to determine the latest recommendations for the management of an overdose of any drug. As rivastigmine has a plasma half-life of about 3.4 hours after patch administration and a duration of acetylcholinesterase inhibition of about 9 hours, it is recommended that in cases of asymptomatic overdose the patch should be immediately removed and no further patch should be applied for the next 24 hours.
As in any case of overdose, general supportive measures should be utilized.
Overdosage with cholinesterase inhibitors can result in cholinergic crisis characterized by severe nausea, vomiting, salivation, sweating, bradycardia, hypotension, respiratory depression, and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved. Atypical responses in blood pressure and heart rate have been reported with other drugs that increase cholinergic activity when coadministered with quaternary anticholinergics such as glycopyrrolate. Additional symptoms associated with rivastigmine overdose are diarrhea, abdominal pain, dizziness, tremor, headache, somnolence, confusional state, hyperhidrosis, hypertension, hallucinations and malaise. Due to the short plasma elimination half-life of rivastigmine after patch administration, dialysis (hemodialysis, peritoneal dialysis, or hemofiltration) would not be clinically indicated in the event of an overdose.
In overdose accompanied by severe nausea and vomiting, the use of antiemetics should be considered. A fatal outcome has rarely been reported with rivastigmine overdose.
11 Description
Rivastigmine Patch (rivastigmine transdermal system) contains rivastigmine, a reversible cholinesterase inhibitor known chemically as (S)- 3-[1-(dimethylamino) ethyl]phenyl ethylmethylcarbamate. It has an empirical formula of C14H22N2O2 as the base and a molecular weight of 250.34 (as the base). Rivastigmine is a viscous, clear, and colorless to yellow to very slightly brown liquid that is sparingly soluble in water and very soluble in ethanol, acetonitrile, n-octanol and ethyl acetate.
The distribution coefficient at 37°C in n-octanol/phosphate buffer solution pH 7 is 4.27.
Rivastigmine Patch is for transdermal administration. The patch comprises a multi-layer laminate containing the coversheet, backing film, reservoir layer, adhesive layer, and release liner as described below. The release liner is removed and discarded prior to use. See Figure 1 for a detailed illustration.
- a cover sheet: siliconised polyethylene terephthalate film
- a backing film: Polyethylene / thermoplastic resin / aluminum coated polyester film
- an active reservoir layer containing the active pharmaceutical ingredient
- an adhesive matrix layer
- a release liner: fluoropolymer coated polyester film
Figure 1: Schematic drawing of Rivastigmine Transdermal System
| Coversheet Backing Film Reservoir Layer Adhesive Layer Release Liner |
Excipients within the formulation include colloidal silicon dioxide, light mineral oil, polyisobutylene adhesive, acrylate-vinylacetate pressure sensitive adhesive, aluminum coated polyester backing.
12.1 Mechanism Of Action
Although the precise mechanism of action of rivastigmine is unknown, it is thought to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine through reversible inhibition of its hydrolysis by cholinesterase. The effect of rivastigmine may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that rivastigmine alters the course of the underlying dementing process.
12.2 Pharmacodynamics
After a 6-mg oral dose of rivastigmine in humans, anticholinesterase activity is present in cerebrospinal fluid for about 10 hours, with a maximum inhibition of about 60% 5 hours after dosing.
In vitro and in vivo studies demonstrate that the inhibition of cholinesterase by rivastigmine is not affected by the concomitant administration of memantine, an N-methyl-D-aspartate receptor antagonist.
12.3 Pharmacokinetics
Absorption
After the initial application of Rivastigmine Patch, there is a lag time of 0.5 to 1 hour in the absorption of rivastigmine. Concentrations then rise slowly typically reaching a maximum after 8 hours, although maximum values (Cmax) can also occur later (at 10 to 16 hours). After the peak, plasma concentrations slowly decrease over the remainder of the 24-hour period of application. At steady state, trough levels are approximately 60% to 80% of peak levels.
Rivastigmine Patch 9.5 mg/24 hours gave exposure approximately the same as that provided by an oral dose of 6 mg twice daily (i.e., 12 mg/day). Inter-subject variability in exposure was lower (43% to 49%) for the Rivastigmine Patch formulation as compared with the oral formulations (73% to 103%). Fluctuation (between Cmax and Cmin) is less for Rivastigmine Patch than for the oral formulation of rivastigmine.
Figure 2 displays rivastigmine plasma concentrations over 24 hours for the 3 available patch strengths.
Figure 2: Rivastigmine Plasma Concentrations Following Dermal 24-Hour Patch Application
Over a 24-hour dermal application, approximately 50% of the drug content of the patch is released from the system.
Exposure (AUC∞) to rivastigmine (and metabolite NAP266-90) was highest when the patch was applied to the upper back, chest, or upper arm. Two other sites (abdomen and thigh) could be used if none of the three other sites is available, but the practitioner should be aware that the rivastigmine plasma exposure associated with these sites was approximately 20 to 30% lower.
There was no relevant accumulation of rivastigmine or the metabolite NAP226-90 in plasma in patients with Alzheimer’s disease with daily dosing.
The pharmacokinetic profile of rivastigmine transdermal patches was comparable in patients with Alzheimer’s disease and in patients with dementia associated with Parkinson’s disease.
Distribution
Rivastigmine is weakly bound to plasma proteins (approximately 40%) over the therapeutic range. It readily crosses the blood-brain barrier, reaching CSF peak concentrations in 1.4 to 2.6 hours. It has an apparent volume of distribution in the range of 1.8 to 2.7 L/kg.
Metabolism
Rivastigmine is extensively metabolized primarily via cholinesterase-mediated hydrolysis to the decarbamylated metabolite NAP226-90. In vitro, this metabolite shows minimal inhibition of acetylcholinesterase (<10%). Based on evidence from in vitro and animal studies, the major cytochrome P450 isoenzymes are minimally involved in rivastigmine metabolism.
The metabolite-to-parent AUC∞ ratio was about 0.7 after Rivastigmine Patch application versus 3.5 after oral administration, indicating that much less metabolism occurred after dermal treatment. Less NAP226-90 is formed following patch application, presumably because of the lack of presystemic (hepatic first pass) metabolism. Based on in vitro studies, no unique metabolic routes were detected in human skin.
Elimination
Renal excretion of the metabolites is the major route of elimination. Unchanged rivastigmine is found in trace amounts in the urine. Following administration of 14C-rivastigmine, renal elimination was rapid and essentially complete (>90%) within 24 hours. Less than 1% of the administered dose is excreted in the feces. The apparent elimination half-life in plasma is approximately 3 hours after patch removal. Renal clearance was approximately 2.1 to 2.8 L/hr.
Age
Age had no impact on the exposure to rivastigmine in Alzheimer’s disease patients treated with Rivastigmine Patch.
Gender and Race
No specific pharmacokinetic study was conducted to investigate the effect of gender and race on the disposition of Rivastigmine Patch. A population pharmacokinetic analysis of oral rivastigmine indicated that neither gender (n=277 males and 348 females) nor race (n=575 Caucasian, 34 Black, 4 Asian, and 12 Other) affected clearance of the drug. Similar results were seen with analyses of pharmacokinetic data obtained after the administration of Rivastigmine Patch.
Body Weight
A relationship between drug exposure at steady state (rivastigmine and metabolite NAP226-90) and body weight was observed in Alzheimer’s dementia patients. Rivastigmine exposure is higher in subjects with low body weight. Compared to a patient with a body weight of 65 kg, the rivastigmine steady-state concentrations in a patient with a body weight of 35 kg would be approximately doubled, while for a patient with a body weight of 100 kg the concentrations would be approximately halved [see Dosage and Administration (2.2)].
Renal Impairment
No study was conducted with Rivastigmine Patch in subjects with renal impairment. Based on population analysis, creatinine clearance did not show any clear effect on steady state concentrations of rivastigmine or its metabolite.
Hepatic Impairment
No pharmacokinetic study was conducted with Rivastigmine Patch in subjects with hepatic impairment. Following a single 3-mg dose, mean oral clearance of rivastigmine was 60% lower in hepatically impaired patients (n=10, biopsy proven) than in healthy subjects (n=10). After multiple 6-mg twice a day oral dosing, the mean clearance of rivastigmine was 65% lower in mild (n=7, Child-Pugh score 5 to 6) and moderate (n=3, Child-Pugh score 7 to 9) hepatically impaired patients (biopsy proven, liver cirrhosis) than in healthy subjects (n=10). [see Dosage and Administration (2.2), Use in Specific Populations (8.6)].
Smoking
Following oral rivastigmine administration (up to 12 mg/day) with nicotine use, population pharmacokinetic analysis showed increased oral clearance of rivastigmine by 23% (n=75 smokers and 549 nonsmokers).
Drug Interaction Studies
No specific interaction studies have been conducted with Rivastigmine Patch. Information presented below is from studies with oral rivastigmine.
Effect of Rivastigmine on the Metabolism of Other Drugs
Rivastigmine is primarily metabolized through hydrolysis by esterases. Minimal metabolism occurs via the major cytochrome P450 isoenzymes. Based on in vitro studies, no pharmacokinetic drug interactions with drugs metabolized by the following isoenzyme systems are expected: CYP1A2, CYP2D6, CYP3A4/5, CYP2E1, CYP2C9, CYP2C8, CYP2C19, or CYP2B6.
No pharmacokinetic interaction was observed between rivastigmine taken orally and digoxin, warfarin, diazepam, or fluoxetine in studies in healthy volunteers. The increase in prothrombin time induced by warfarin is not affected by administration of rivastigmine.
Effect of Other Drugs on the Metabolism of Rivastigmine
Drugs that induce or inhibit CYP450 metabolism are not expected to alter the metabolism of rivastigmine.
Population pharmacokinetic analysis with a database of 625 patients showed that the pharmacokinetics of rivastigmine taken orally were not influenced by commonly prescribed medications such as antacids (n=77), antihypertensives (n=72), beta-blockers (n=42), calcium channel blockers (n=75), antidiabetics (n=21), nonsteroidal anti-inflammatory drugs (n=79), estrogens (n=70), salicylate analgesics (n=177), antianginals (n=35), and antihistamines (n=15).
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Carcinogenesis
In oral carcinogenicity studies conducted at doses up to 1.1 mg base/kg/day in rats and 1.6 mg base/kg/day in mice, rivastigmine was not carcinogenic.
In a dermal carcinogenicity study conducted at doses up to 0.75 mg base/kg/day in mice, rivastigmine was not carcinogenic. The mean rivastigmine plasma exposure (AUC) at this dose was less than that in humans at the maximum recommended human dose (13.3 mg/24 hours).
Mutagenesis
Rivastigmine was clastogenic in in vitro chromosomal aberration assays in mammalian cells in the presence, but not the absence, of metabolic activation. Rivastigmine was negative in an in vitro bacterial reverse mutation (Ames) assay, an in vitro HGPRT assay, and in an in vivo mouse micronucleus test.
Impairment of Fertility
No fertility or reproduction studies of dermal rivastigmine have been conducted in animals. Rivastigmine had no effect on fertility or reproductive performance in rats at oral doses up to 1.1 mg base/kg/day.
14 Clinical Studies
The effectiveness of the Rivastigmine Patch in dementia of the Alzheimer’s type and dementia associated with Parkinson’s disease was based on the results of controlled trials of Rivastigmine Patch in patients with Alzheimer’s disease (Studies 1 and 2) (see below); 3 controlled trials of oral rivastigmine in patients with dementia of the Alzheimer’s type; and 1 controlled trial of oral rivastigmine in patients with dementia associated with Parkinson’s disease. See the prescribing information for oral rivastigmine for details of the four studies of oral rivastigmine.
Mild to Moderate Alzheimer’s Disease
International 24-Week Study of Rivastigmine Patch in Dementia of the Alzheimer’s Type (Study 1)
This study was a randomized double-blind, double dummy clinical investigation in patients with Alzheimer’s disease [diagnosed by NINCDS-ADRDA and DSM-IV criteria, Mini-Mental Status Examination (MMSE) score ≥10 and ≤20] (Study 1). The mean age of patients participating in this trial was 74 years with a range of 50 to 90 years. Approximately 67% of patients were women, and 33% were men. The racial distribution was Caucasian 75%, Black 1%, Asian 9%, and other races 15%.
The effectiveness of the Rivastigmine Patch was evaluated in Study 1 using a dual outcome assessment strategy, evaluating for changes in both cognitive performance and overall clinical effect.
The ability of the Rivastigmine Patch to improve cognitive performance was assessed with the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-Cog), a multi-item instrument that has been extensively validated in longitudinal cohorts of Alzheimer’s disease patients. The ADAS-Cog examines selected aspects of cognitive performance including elements of memory, orientation, attention, reasoning, language, and praxis. The ADAS-Cog scoring range is from 0 to 70, with higher scores indicating greater cognitive impairment. Elderly normal adults may score as low as 0 or 1, but it is not unusual for non-demented adults to score slightly higher.
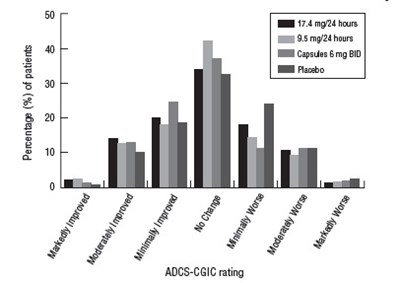
The ability of the Rivastigmine Patch to produce an overall clinical effect was assessed using the Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change (ADCS-CGIC). The ADCS-CGIC is a more standardized form of the Clinician's Interview-Based Impression Of Change-Plus (CIBIC-Plus) and is also scored as a 7-point categorical rating; scores range from 1, indicating “markedly improved,” to 4, indicating “no change,” to 7, indicating “marked worsening.”
In Study 1, 1195 patients were randomized to 1 of the following 4 treatments: Rivastigmine Patch 9.5 mg/24 hours, Rivastigmine Patch 17.4 mg/24 hours, rivastigmine capsules in a dose of 6 mg twice daily, or placebo. This 24-week study was divided into a 16-week titration phase followed by an 8-week maintenance phase. In the active treatment arms of this study, doses below the target dose were permitted during the maintenance phase in the event of poor tolerability.
Figure 3 illustrates the time course for the change from baseline in ADAS-Cog scores for all 4 treatment groups over the 24-week study. At 24 weeks, the mean differences in the ADAS-Cog change scores for the rivastigmine-treated patients compared to the patients on placebo, were 1.8, 2.9, and 1.8 units for the Rivastigmine Patch 9.5 mg/24 hours, Rivastigmine Patch 17.4 mg/24 hours, and rivastigmine capsule 6 mg twice daily groups, respectively. The difference between each of these groups and placebo was statistically significant. Although a slight improvement was observed with the 17.4 mg/24 hours patch compared to the 9.5 mg/24 hours patch on this outcome measure, no meaningful difference between the two was seen on the global evaluation (see Figure 4)
Figure 3: Time Course of the Change from Baseline in ADAS-Cog Score for Patients Observed at Each Time Point in Study 1
Figure 4 presents the distribution of patients’ scores on the ADCS-CGIC for all 4 treatment groups. At 24 weeks, the mean difference in the ADCS-CGIC scores for the comparison of patients in each of the rivastigmine-treated groups with the patients on placebo was 0.2 units. The difference between each of these groups and placebo was statistically significant.
Figure 4: Distribution of ADCS-CGIC Scores for Patients Completing Study 1
International 48-Week Study of Rivastigmine Patch in Dementia of the Alzheimer’s Type (Study 2)
This study was a randomized double-blind clinical investigation in patients with Alzheimer’s disease [diagnosed by NINCDS-ADRDA and DSM-IV criteria, Mini-Mental State Examination (MMSE) score ≥10 and ≤24] (Study 2). The mean age of patients participating in this trial was 76 years with a range of 50 to 85 years. Approximately 65% of patients were women and 35% were men. The racial distribution was approximately Caucasian 97%, Black 2%, Asian 0.5% and other races 1%. Approximately 27% of the patients were taking memantine throughout the entire duration of the study.
Alzheimer’s disease patients who received 24 to 48 weeks open label treatment with Rivastigmine Patch 9.5 mg/24 hours and who demonstrated functional and cognitive decline were randomized into treatment with either Rivastigmine Patch 9.5 mg/24 hours or Rivastigmine Patch 13.3 mg/24 hours in a 48-week, double blind treatment phase. Functional decline was assessed by the investigator and cognitive decline was defined as a decrease in the MMSE score of ≥2 points from the previous visit or a decrease of ≥3 points from baseline.
Study 2 was designed to compare the efficacy of Rivastigmine Patch 13.3 mg/24 hours versus that of Rivastigmine Patch 9.5 mg/24 hours during the 48-week double blind treatment phase.
The ability of the Rivastigmine Patch 13.3 mg/24 hours to improve cognitive performance over that provided by the Rivastigmine Patch 9.5 mg/24 hours was assessed by the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-Cog) [see Clinical Studies, International 24-Week Study (14)].
The ability of the Rivastigmine Patch 13.3 mg/24 hours to improve overall function versus that provided by Rivastigmine Patch 9.5 mg/24 hours was assessed by the instrumental subscale of the Alzheimer’s Disease Cooperative Study Activities of Daily Living (ADCS-IADL). The ADCS-IADL subscale is composed of items 7 to 23 of the caregiver-based ADCS-ADL scale. The ADCS-IADL assesses activities such as those necessary for communicating and interacting with other people, maintaining a household, and conducting hobbies and interests. A sum score is calculated by adding the scores of the individual items and can range from 0 to 56, with higher scores indicating less impairment.
Out of a total of 1584 patients enrolled in the initial open-label phase of the study, 567 patients were classified as decliners and were randomized into the 48-week double-blind treatment phase of the study. Two hundred eighty-seven (287) patients entered the 9.5 mg/24 hours Rivastigmine Patch treatment group and 280 patients entered the 13.3 mg/24 hours Rivastigmine Patch treatment group.
Figure 5 illustrates the time course for the mean change from double-blind baseline in ADCS-IADL scores for each treatment group over the course of the 48-week treatment phase of the study. Decline in the mean ADCS-IADL score from the double-blind baseline for the Intent to Treat–Last Observation Carried Forward (ITT-LOCF) analysis was less at each timepoint in the 13.3 mg/24 hour Rivastigmine Patch treatment group than in the 9.5 mg/24 hours Rivastigmine Patch treatment group. The 13.3 mg/24 hours dose was statistically significantly superior to the 9.5 mg/24 hours dose at weeks 16, 24, 32, and 48 (primary endpoint).
Figure 6 illustrates the time course for the mean change from double-blind baseline in ADAS-Cog scores for both treatment groups over the 48-week treatment phase. The between-treatment group difference for Rivastigmine Patch 13.3 mg/24 hours versus Rivastigmine Patch 9.5 mg/24 hours was nominally statistically significant at week 24 (p=0.027), but not at week 48 (p=0.227), which was the primary endpoint.
Figure 5: Time Course of the Change from Double-Blind Baseline in ADCS-IADL Score for Patients Observed at Each Time Point in Study 2
Figure 6: Time Course of the Change from Double-Blind Baseline in ADAS-Cog Score for Patients Observed at Each Time Point in Study 2
16 How Supplied/Storage And Handling
Rivastigmine Patch: 4.6 mg/24 hours
Each patch of 4.6 cm2 contains 6.9 mg rivastigmine with in vivo release rate of 4.6 mg/24 hours.
Carton of 30………………………NDC 47781-304-03
Rivastigmine Patch: 9.5 mg/24 hours
Each patch of 9.2 cm2 contains 13.8 mg rivastigmine with in vivo release rate of 9.5 mg/24 hours.
Carton of 30………………………NDC 47781-305-03
Rivastigmine Patch: 13.3 mg/24 hours
Each patch of 13.8 cm2 contains 20.7 mg rivastigmine with in vivo release rate of 13.3 mg/24 hours.
Carton of 30………………………NDC 47781-405-03
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Keep Rivastigmine Patch in the individual sealed pouch until use. Each pouch contains 1 patch. Used systems should be folded, with the adhesive surfaces pressed together, and discarded safely.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Importance of Correct Usage
Inform patients or caregivers of the importance of applying the correct dose on the correct part of the body. They should be instructed to rotate the application site in order to minimize skin irritation. The same site should not be used within 14 days. The previous day’s patch must be removed before applying a new patch to a different skin location. Rivastigmine Patch should be replaced every 24 hours and the time of day should be consistent. It may be helpful for this to be part of a daily routine, such as the daily bath or shower. Only 1 patch should be worn at a time.
Instruct patients or caregivers to avoid exposure of the patch to external heat sources (excessive sunlight, saunas, solariums) for long periods of time.
Instruct patients who have missed a dose to apply a new patch immediately. They may apply the next patch at the usual time the next day. Instruct patients to not apply 2 patches to make up for 1 missed.
Inform the patient or caregiver to contact the physician for retitration instructions if treatment has been interrupted.
Discarding Used Patches
Instruct patients or caregivers to fold the patch in half after use, return the used patch to its original pouch, and discard it out of the reach and sight of children and pets. They should also be informed that drug still remains in the patch after 24-hour usage. They should be instructed to avoid eye contact and to wash their hands after handling the patch. In case of accidental contact with the eyes, or if their eyes become red after handling the patch, they should be instructed to rinse immediately with plenty of water and to seek medical advice if symptoms do not resolve.
Gastrointestinal Adverse Reactions
Inform patients or caregivers of the potential gastrointestinal adverse reactions such as nausea, vomiting, and diarrhea, including the possibility of dehydration due to these symptoms. Explain that Rivastigmine Patch may affect the patient’s appetite and/or the patient’s weight. Patients and caregivers should be instructed to look for these adverse reactions, in particular when treatment is initiated or the dose is increased. Instruct patients and caregivers to inform a physician if these adverse reactions persist.
Skin Reactions
Inform patients or caregivers about the potential for allergic contact dermatitis reactions to occur. Patients or caregivers should be instructed to inform a physician if application site reactions spread beyond the patch size, if there is evidence of a more intense local reaction (e.g., increasing erythema, edema, papules, vesicles) and if symptoms do not significantly improve within 48 hours after patch removal.
Concomitant Use of Drugs with Cholinergic Action
Inform patients or caregivers that while wearing Rivastigmine Patch, patients should not be taking rivastigmine capsules or rivastigmine oral solution or other drugs with cholinergic effects.
Patient Information
Rivastigmine (riv” a stig’ meen) Patch
(rivastigmine transdermal system)
Rivastigmine Patch is for skin use only.
What is Rivastigmine Patch?
Rivastigmine Patch is a prescription medicine used to treat:
Mild to moderate memory problems (dementia) associated with Alzheimer’s disease.
- Mild to moderate memory problems (dementia) associated with Parkinson’s disease.
- Seem much better
- Get better in small ways or stay the same
- Get worse but slower than expected
- Not change and then get worse as expected
- are allergic to rivastigmine, carbamate derivatives, or any of the ingredients in Rivastigmine Patch. See the end of this leaflet for a complete list of ingredients in Rivastigmine Patch.
- have had a skin reaction that:
- spread beyond the Rivastigmine Patch size
- had blisters, increased skin redness, or swelling
- did not get better within 48 hours after you removed the Rivastigmine Patch
- have or have had a stomach ulcer
- are planning to have surgery
- have or have had problems with your heart
- have problems passing urine
- have or have had seizures
- have problems with movement (tremors)
- have asthma or breathing problems
- have a loss of appetite or are losing weight
- have had a skin reaction to rivastigmine (the medicine in Rivastigmine Patch) in the past.
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if the medicine in Rivastigmine Patch will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. It is not known if the medicine in Rivastigmine Patch passes into your breast milk. You and your healthcare provider should decide if you will use Rivastigmine Patch or breastfeed. You should not do both.
- a medicine used to treat inflammation [nonsteroidal anti-inflammatory drugs (NSAIDS)]
- other medicines used to treat Alzheimer’s or Parkinson’s disease
- an anticholinergic medicine, such as an allergy or cold medicine, a medicine to treat bladder or bowel spasms, or certain asthma medicines, or certain medicines to prevent motion or travel sickness
- metoclopramide, a drug given to relieve symptoms of nausea, gastroesophageal reflux disease (GERD), or nausea and vomiting after surgery or chemotherapy treatment
- If you are undergoing surgery while using Rivastigmine Patch, inform your doctor because Rivastigmine Patch may exaggerate the effects of anesthesia, or the effects of a beta-blocker, a type of medicine given for high blood pressure, heart disease, and other medical conditions
- Use Rivastigmine Patch exactly as your healthcare provider tells you to use it.
- Rivastigmine Patch comes in 3 different dosage strengths.
- Your healthcare provider may change your dose as needed.
- Wear only 1 Rivastigmine Patch at a time.
- Rivastigmine Patch is for skin use only.
- Only apply Rivastigmine Patch to healthy skin that is clean, dry, hairless, and free of redness, irritation, burns or cuts.
- Avoid applying Rivastigmine Patch to areas on your body that will be rubbed against by tight clothing.
- Do not apply Rivastigmine Patch to skin that has cream, lotion, or powder on it.
- Change your Rivastigmine Patch every 24 hours at the same time of day. You may write the date and time you put on the Rivastigmine Patch with a ballpoint pen before applying the patch to help you remember when to remove it.
- Change your application site every day to avoid skin irritation. You can use the same area, but do not use the exact same spot for at least 14 days after your last application.
- Check to see if the Rivastigmine Patch has become loose when you are bathing, swimming, or showering.
- Rivastigmine Patch is designed to deliver medication during the time it is worn. If your Rivastigmine Patch falls off before its usual replacement time, put on a new Rivastigmine Patch right away. Replace the new patch the next day at the same time as usual. Do not use overlays, bandages, or tape to secure Rivastigmine Patch that has become loose or try to reapply a Rivastigmine Patch that has fallen off.
- If you miss a dose or forget to change your Rivastigmine Patch apply your next Rivastigmine Patch as soon as you remember. Do not apply 2 Rivastigmine Patches to make up for the missed dose.
- If you miss more than 3 doses of applying Rivastigmine Patch, call your healthcare provider before putting on a new Rivastigmine Patch. You may need to restart Rivastigmine Patch at a lower dose.
- Always remove the old Rivastigmine Patch from the previous day before you apply a new one.
- Having more than 1 Rivastigmine Patch on your body at the same time can cause you to get too much medicine. If you accidentally use more than 1 Rivastigmine Patch at a time, call your healthcare provider right away. If you are unable to reach your healthcare provider, call your local Poison Control Center at 1-800-222-1222 or go to the nearest hospital emergency room right away.
- Do not touch your eyes after you touch the Rivastigmine Patch. In case of accidental contact with your eyes or if your eyes become red after handling the patch, rinse immediately with plenty of water and seek medical advice if symptoms do not resolve.
- Rivastigmine Patch can cause drowsiness, dizziness, weakness, or fainting. Do not drive, operate heavy machinery, or do other dangerous activities until you know how Rivastigmine Patch affects you.
- Avoid exposure to heat sources such as excessive sunlight, saunas, or sunrooms for long periods of time.
- Skin burns have been reported at the patch site in several patients wearing an aluminized transdermal system during a Magnetic Resonance Imaging scan (MRI). Because the Rivastigmine Patch contains aluminum, it is recommended to remove the system before undergoing an MRI.
- Medication overdose. Hospitalization and rarely death may happen when people accidently wear more than 1 patch at the same time. It is important that the old Rivastigmine Patch be removed before you apply a new one. Do not wear more than 1 Rivastigmine Patch at a time.
- Stomach or bowel (intestinal) problems, including:
- nausea
- vomiting
- diarrhea
- dehydration
- loss of appetite
- weight loss
- bleeding in your stomach (ulcers)
- Skin reactions. Some people have had a serious skin reaction called allergic contact dermatitis (ACD) when using Rivastigmine Patch. Stop using Rivastigmine Patch and call your healthcare provider right away if you experience reactions that spread beyond the patch size, are intense in nature and do not improve within 48 hours after the patch is removed. Symptoms of ACD may be intense and include:
- itching, redness, swelling, warmth or tenderness of the skin
- peeling or blistering of the skin that may ooze, drain or crust over
- heart problems
- seizures
- problems with movement (tremors)
- depression
- headache
- anxiety
- dizziness
- stomach pain
- urinary tract infections
- muscle weakness
- triedness
- trouble sleeping
- Store Rivastigmine Patch at 59° F to 86°F (15°C to 30°C).
- Keep Rivastigmine Patch in the sealed pouch until ready to use.
Based on clinical trials conducted over 6 to 12 months Rivastigmine Patch was shown to help with cognition which includes (memory, understanding communication, reasoning) and with doing daily tasks. Rivastigmine Patch does not work the same in all people. Some people treated with Rivastigmine Patch may:
Some patients will not benefit from treatment with Rivastigmine Patch. Rivastigmine Patch does not cure Alzheimer’s disease. All patients with Alzheimer’s disease get worse over time.
Rivastigmine Patch comes as a transdermal system that delivers rivastigmine (the medicine in Rivastigmine Patch) through the skin.
It is not known if Rivastigmine Patch is safe or effective in children under 18 years of age.
Who should not use Rivastigmine Patch?
Do not use Rivastigmine Patch if you:
Ask your healthcare provider if you are not sure if you should use Rivastigmine Patch.
What should I tell my healthcare provider before using Rivastigmine Patch?
Before you use Rivastigmine Patch, tell your healthcare provider if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Especially tell your healthcare provider if you take:
Ask your healthcare provider if you are not sure if your medicine is one listed above.
Know the medicines you take. Keep a list of them to show to your healthcare provider and pharmacist when you get a new medicine.
How should I use Rivastigmine Patch?
What should I avoid while using Rivastigmine Patch?
What are the possible side effects of Rivastigmine Patch?
Rivastigmine Patch may cause serious side effects, including:
The most common side effects of Rivastigmine Patch include:
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Rivastigmine Patch. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store Rivastigmine Patch?
Keep Rivastigmine Patch and all medicines out of the reach of children.
General information about the safe and effective use of Rivastigmine Patch.
Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use Rivastigmine Patch for a condition for which it was not prescribed. Do not give Rivastigmine Patch to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about Rivastigmine Patch. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about Rivastigmine Patch that is written for health professionals.
For more information, contact Alvogen at 1-866-770-3024.
What are the ingredients of Rivastigmine Patch?
Active ingredient: rivastigmine
Excipients include: colloidal silicon dioxide, light mineral oil, polyisobutylene adhesive, acrylate-vinylacetate pressure sensitive adhesive, aluminum coated polyester backing
Made in Germany
Distributed by:
Alvogen, Inc.
Pine Brook, NJ 07058 USA
PL304-04
12/2016
Instructions For Use
Rivastigmine (riv” a stig’ meen) Patch
(rivastigmine transdermal system)
You will need the following supplies (See Figure A):
Rivastigmine Patch is supplied in cartons containing 30 patches (see Figure A)
Figure A
- Rivastigmine Patch is a thin, tan, plastic patch that sticks to the skin. Each Rivastigmine Patch is sealed in a pouch that protects it until you are ready to put it on. (See Figure A).
- Only 1 Rivastigmine Patch should be worn at a time. Do not apply more than 1 Rivastigmine Patch at a time to the body.
- Do not open the pouch or remove the Rivastigmine Patch until you are ready to apply it.
- Instructions for Caregivers: Apply Rivastigmine Patch to the upper or lower back if it is likely that the patient will remove it. If this is not a concern, the Rivastigmine Patch can be applied instead to the upper arm or chest. Do not apply the Rivastigmine Patch to areas where it can be rubbed off by tight clothing or belts.
- Only apply the Rivastigmine Patch to healthy skin that is clean, dry, hairless, and free of redness, irritation, burns or cuts.
- Do not cut or fold the Rivastigmine Patch itself.
- A protective liner covers the sticky (adhesive) side of the Rivastigmine Patch. Peel off 1 side of the protective liner. Do not touch the sticky part of the Rivastigmine Patch with your fingers.
- Apply the sticky (adhesive) side of the Rivastigmine Patch onto your chosen area of skin and then peel off the other side of the protective liner as well as the cover sheet and discard both.
- Press down on the Rivastigmine Patch firmly for 30 seconds to make sure that the edges stick to your skin (See Figure F).
- If your Rivastigmine Patch falls off, select a new area, and repeat Steps 2 to 5 to apply a new Rivastigmine Patch.
- Be sure to replace the new Rivastigmine Patch the next day at the same time as usual.
- Gently pull on 1 edge of the Rivastigmine Patch to remove it from your skin.
- Fold the Rivastigmine Patch in half (with the sticky sides together) and put it back into the pouch that you saved.
- Throw away the used Rivastigmine Patch safely and out of the reach of children and pets.
- Some medicine stays in the patch for 24 hours after you use it and should be folded together (sticky side together) and safely thrown away. Do not try to re-use Rivastigmine Patches.
- After you remove the Rivastigmine patch, if any adhesive remains on your skin, you can use soap and water or an oil-based substance (such as baby oil) to remove the adhesive. Alcohol or other dissolving liquids (such as nail polish remover) should not be used.
Using Rivastigmine Patch:
Step 1. Choose an area to apply the Rivastigmine Patch (See Figure B).
Figure B
The diagram represents areas on the body where Rivastigmine Patch may be applied. Only 1 patch should be worn at a time. Do not apply multiple patches to the body.
Step 2. Remove the Rivastigmine Patch from the pouch (See Figure C).
Carefully cut the pouch along the dotted line to open and remove the Rivastigmine Patch. Save the pouch for later use.
Figure C
Step 3. Remove 1 side of the adhesive liner (See Figure D).
Figure D
Step 4. Apply the Rivastigmine Patch to your skin (See Figure E).
Figure E
Figure F
Step 5: Wash your hands with soap and water right away.
Note:
Removing the Rivastigmine Patch:
Step 6. Remove the Rivastigmine Patch from the skin (See Figure G).Figure G
Throwing away the used Rivastigmine Patch:
Step 7. Throw away the used Rivastigmine Patch (See Figure H).
Figure H
Step 8: Wash your hands with soap and water right away.
This Patient Information and Instructions for Use have been approved by the U.S. Food and Drug Administration.
Made in Germany
Distributed by:
Alvogen, Inc.
Pine Brook, NJ 07058 USA
PL304-04
12/2016
Carton - 4.6 Mg/24 Hours
NDC 47781-304-03 Rx only
RIVASTIGMINE
TRANSDERMAL
SYSTEM
Delivers 4.6mg/24 hours
For Transdermal Use Only.
To avoid possible burns, remove Rivastigmine
Transdermal System before undergoing an
MRI (magnetic resonance imaging) procedure.
Contains 30 Systems
Pouch - 4.6 Mg/24 Hours
NDC 47781-304-11
Rivastigmine Transdermal System
Delivers 4.6 mg/24 hours
Carton - 9.5 Mg/24 Hours
NDC 47781-305-03 Rx only
RIVASTIGMINE
TRANSDERMAL
SYSTEM
Delivers 9.5 mg/24 hours
For Transdermal Use Only.
To avoid possible burns, remove Rivastigmine
Transdermal System before undergoing an
MRI (magnetic resonance imaging) procedure.
Contains 30 Systems
Pouch - 9.5 Mg/24 Hours
NDC 47781-305-11
Rivastigmine Transdermal System
Delivers 9.5 mg/24 hours
Carton - 13.3 Mg/24 Hours
NDC 47781-405-03 Rx only
RIVASTIGMINE
TRANSDERMAL
SYSTEM
Delivers 13.3 mg/24 hours
For Transdermal Use Only.
To avoid possible burns, remove Rivastigmine
Transdermal System before undergoing an
MRI (magnetic resonance imaging) procedure.
Contains 30 Systems
Pouch - 13.3 Mg/24 Hours
NDC 47781-405-11
Rivastigmine Transdermal System
Delivers 13.3 mg/24 hours
* Please review the disclaimer below.