FDA Label for Teriparatide
View Indications, Usage & Precautions
- WARNING: POTENTIAL RISK OF OSTEOSARCOMA
- 1.1 TREATMENT OF POSTMENOPAUSAL WOMEN WITH OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 1.2 INCREASE OF BONE MASS IN MEN WITH PRIMARY OR HYPOGONADAL OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 1.3 TREATMENT OF MEN AND WOMEN WITH GLUCOCORTICOID-INDUCED OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 2.1 TREATMENT OF POSTMENOPAUSAL WOMEN WITH OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 2.2 INCREASE OF BONE MASS IN MEN WITH PRIMARY OR HYPOGONADAL OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 2.3 TREATMENT OF MEN AND WOMEN WITH GLUCOCORTICOID-INDUCED OSTEOPOROSIS AT HIGH RISK FOR FRACTURE
- 2.4 ADMINISTRATION
- 2.5 TREATMENT DURATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5.1 OSTEOSARCOMA
- 5.2 TREATMENT DURATION
- 5.3 BONE METASTASES AND SKELETAL MALIGNANCIES
- 5.4 METABOLIC BONE DISEASES
- 5.5 HYPERCALCEMIA AND HYPERCALCEMIC DISORDERS
- 5.6 UROLITHIASIS OR PRE-EXISTING HYPERCALCIURIA
- 5.7 ORTHOSTATIC HYPOTENSION
- 5.8 DRUG INTERACTIONS
- 6.1 CLINICAL TRIALS EXPERIENCE
- OTHER
- 6.2 POSTMARKETING EXPERIENCE
- 6.3 IMMUNOGENICITY
- 7.1 DIGOXIN
- 7.2 HYDROCHLOROTHIAZIDE
- 7.3 FUROSEMIDE
- 8.1 PREGNANCY
- 8.2 LACTATION
- 8.4 PEDIATRIC USE
- 8.5 GERIATRIC USE
- 8.6 HEPATIC IMPAIRMENT
- 8.7 RENAL IMPAIRMENT
- 10 OVERDOSAGE
- 11 DESCRIPTION
- 12.1 MECHANISM OF ACTION
- 12.2 PHARMACODYNAMICS
- 12.3 PHARMACOKINETICS
- 13.1 CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
- 13.2 ANIMAL TOXICOLOGY AND/OR PHARMACOLOGY
- 14.1 TREATMENT OF OSTEOPOROSIS IN POSTMENOPAUSAL WOMEN
- 14.2 TREATMENT TO INCREASE BONE MASS IN MEN WITH PRIMARY OR HYPOGONADAL OSTEOPOROSIS
- 14.3 TREATMENT OF MEN AND WOMEN WITH GLUCOCORTICOID-INDUCED OSTEOPOROSIS
- 16.1 HOW SUPPLIED
- 16.2 STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- 17.1 POTENTIAL RISK OF OSTEOSARCOMA
- 17.2 ORTHOSTATIC HYPOTENSION
- 17.3 HYPERCALCEMIA
- 17.4 OTHER OSTEOPOROSIS TREATMENT MODALITIES
- 17.5 USE OF DELIVERY DEVICE (PEN)
- 17.6 AVAILABILITY OF MEDICATION GUIDE AND USER MANUAL
- SPL MEDGUIDE
- PREPARE FOR INJECTION
- ADMINISTER INJECTION
- AFTER INJECTION
- TROUBLESHOOTING
- DISPOSAL INFORMATION
- CLEANING AND STORAGE
- OTHER IMPORTANT NOTES
- DISPOSAL OF PEN NEEDLES AND DELIVERY DEVICE
- CONTACT INFORMATION
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL SECTION
Teriparatide Product Label
The following document was submitted to the FDA by the labeler of this product Alvogen, Inc.. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
Warning: Potential Risk Of Osteosarcoma
In male and female rats, teriparatide caused an increase in the incidence of osteosarcoma (a malignant bone tumor) that was dependent on dose and treatment duration. The effect was observed at systemic exposures to teriparatide ranging from 3 to 60 times the exposure in humans given a 20 mcg dose. Because of the uncertain relevance of the rat osteosarcoma finding to humans, prescribe teriparatide injection only for patients for whom the potential benefits are considered to outweigh the potential risk. Teriparatide injection should not be prescribed for patients who are at increased baseline risk for osteosarcoma (including those with Paget's disease of bone or unexplained elevations of alkaline phosphatase, pediatric and young adult patients with open epiphyses, or prior external beam or implant radiation therapy involving the skeleton) [see Warnings and Precautions (5.1), Adverse Reactions (6.2), and Nonclinical Toxicology (13.1)].
1.1 Treatment Of Postmenopausal Women With Osteoporosis At High Risk For Fracture
Teriparatide injection is indicated for the treatment of postmenopausal women with osteoporosis at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy. In postmenopausal women with osteoporosis, teriparatide injection reduces the risk of vertebral and nonvertebral fractures [see Clinical Studies (14.1)].
1.2 Increase Of Bone Mass In Men With Primary Or Hypogonadal Osteoporosis At High Risk For Fracture
Teriparatide injection is indicated to increase bone mass in men with primary or hypogonadal osteoporosis at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy [see Clinical Studies (14.2)].
1.3 Treatment Of Men And Women With Glucocorticoid-Induced Osteoporosis At High Risk For Fracture
Teriparatide injection is indicated for the treatment of men and women with osteoporosis associated with sustained systemic glucocorticoid therapy (daily dosage equivalent to 5 mg or greater of prednisone) at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy [see Clinical Studies (14.3)].
2.1 Treatment Of Postmenopausal Women With Osteoporosis At High Risk For Fracture
The recommended dose is 20 mcg subcutaneously once a day.
2.2 Increase Of Bone Mass In Men With Primary Or Hypogonadal Osteoporosis At High Risk For Fracture
The recommended dose is 20 mcg subcutaneously once a day.
2.3 Treatment Of Men And Women With Glucocorticoid-Induced Osteoporosis At High Risk For Fracture
The recommended dose is 20 mcg subcutaneously once a day.
2.4 Administration
- Teriparatide injection should be administered as a subcutaneous injection into the thigh or abdominal wall. There are no data available on the safety or efficacy of intravenous or intramuscular injection of teriparatide.
- Teriparatide injection should be administered initially under circumstances in which the patient can sit or lie down if symptoms of orthostatic hypotension occur [see Warnings and Precautions (5.7)].
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Teriparatide injection is a clear and colorless liquid. Do not use if solid particles appear or if the solution is cloudy or colored.
- Patients and caregivers who administer teriparatide injection should receive appropriate training and instruction on the proper use of the teriparatide injection delivery device from a qualified health professional [see Patient Counseling Information (17.5)].
2.5 Treatment Duration
The safety and efficacy of teriparatide have not been evaluated beyond 2 years of treatment. Consequently, use of the drug for more than 2 years during a patient's lifetime is not recommended.
3 Dosage Forms And Strengths
Injection: 620 mcg/2.48 mL (250 mcg/mL)
Colorless solution in a single-patient-use pen containing 28 daily doses of 20 mcg.
4 Contraindications
Teriparatide injection is contraindicated in patients with:
- Hypersensitivity to teriparatide or to any of its excipients. Reactions have included angioedema and anaphylaxis [see Adverse Reactions (6.2)].
5.1 Osteosarcoma
In male and female rats, teriparatide caused an increase in the incidence of osteosarcoma (a malignant bone tumor) that was dependent on dose and treatment duration [see Boxed Warning and Nonclinical Toxicology (13.1)]. Teriparatide injection should not be prescribed for patients at increased baseline risk of osteosarcoma.
These include:
- Paget's disease of bone. Unexplained elevations of alkaline phosphatase may indicate Paget's disease of bone.
- Pediatric and young adult patients with open epiphyses.
- Prior external beam or implant radiation therapy involving the skeleton.
5.2 Treatment Duration
The safety and efficacy of teriparatide have not been evaluated beyond 2 years of treatment. Consequently, use of the drug for more than 2 years during a patients' lifetime is not recommended.
5.3 Bone Metastases And Skeletal Malignancies
Patients with bone metastases or a history of skeletal malignancies should not be treated with teriparatide injection.
5.4 Metabolic Bone Diseases
Patients with metabolic bone diseases other than osteoporosis should not be treated with teriparatide injection.
5.5 Hypercalcemia And Hypercalcemic Disorders
Teriparatide has not been studied in patients with pre-existing hypercalcemia. These patients should not be treated with teriparatide because of the possibility of exacerbating hypercalcemia. Patients known to have an underlying hypercalcemic disorder, such as primary hyperparathyroidism, should not be treated with teriparatide injection.
5.6 Urolithiasis Or Pre-Existing Hypercalciuria
In clinical trials, the frequency of urolithiasis was similar in patients treated with teriparatide and placebo. However, teriparatide has not been studied in patients with active urolithiasis. If active urolithiasis or pre-existing hypercalciuria are suspected, measurement of urinary calcium excretion should be considered. Teriparatide injection should be used with caution in patients with active or recent urolithiasis because of the potential to exacerbate this condition.
5.7 Orthostatic Hypotension
Teriparatide injection should be administered initially under circumstances in which the patient can sit or lie down if symptoms of orthostatic hypotension occur. In short-term clinical pharmacology studies with teriparatide, transient episodes of symptomatic orthostatic hypotension were observed in 5% of patients. Typically, an event began within 4 hours of dosing and spontaneously resolved within a few minutes to a few hours. When transient orthostatic hypotension occurred, it happened within the first several doses, it was relieved by placing the person in a reclining position, and it did not preclude continued treatment.
5.8 Drug Interactions
Hypercalcemia may predispose patients to digitalis toxicity. Because teriparatide transiently increases serum calcium, patients receiving digoxin should use teriparatide injection with caution [see Drug Interactions (7.1) and Clinical Pharmacology (12.2)].
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Other
Treatment of Osteoporosis in Men and Postmenopausal Women
The safety of teriparatide in the treatment of osteoporosis in men and postmenopausal women was assessed in two randomized, double-blind, placebo-controlled trials of 1382 patients (21% men, 79% women) aged 28 to 86 years (mean 67 years). The median durations of the trials were 11 months for men and 19 months for women, with 691 patients exposed to teriparatide and 691 patients to placebo. All patients received 1000 mg of calcium plus at least 400 IU of vitamin D supplementation per day.
The incidence of all cause mortality was 1% in the teriparatide group and 1% in the placebo group. The incidence of serious adverse events was 16% in teriparatide patients and 19% in placebo patients. Early discontinuation due to adverse events occurred in 7% of teriparatide patients and 6% of placebo patients.
Table 1 lists adverse events from the two principal osteoporosis trials in men and postmenopausal women that occurred in ≥2% of teriparatide-treated and more frequently than placebo-treated patients.
| Teriparatide N=691 | Placebo N=691 | |
| Event Classification | (%) | (%) |
| Body as a Whole | ||
| Pain | 21.3 | 20.5 |
| Headache | 7.5 | 7.4 |
| Asthenia | 8.7 | 6.8 |
| Neck pain | 3.0 | 2.7 |
| Cardiovascular | ||
| Hypertension | 7.1 | 6.8 |
| Angina pectoris | 2.5 | 1.6 |
| Syncope | 2.6 | 1.4 |
| Digestive System | ||
| Nausea | 8.5 | 6.7 |
| Constipation | 5.4 | 4.5 |
| Diarrhea | 5.1 | 4.6 |
| Dyspepsia | 5.2 | 4.1 |
| Vomiting | 3.0 | 2.3 |
| Gastrointestinal disorder | 2.3 | 2.0 |
| Tooth disorder | 2.0 | 1.3 |
| Musculoskeletal | ||
| Arthralgia | 10.1 | 8.4 |
| Leg cramps | 2.6 | 1.3 |
| Nervous System | ||
| Dizziness | 8.0 | 5.4 |
| Depression | 4.1 | 2.7 |
| Insomnia | 4.3 | 3.6 |
| Vertigo | 3.8 | 2.7 |
| Respiratory System | ||
| Rhinitis | 9.6 | 8.8 |
| Cough increased | 6.4 | 5.5 |
| Pharyngitis | 5.5 | 4.8 |
| Dyspnea | 3.6 | 2.6 |
| Pneumonia | 3.9 | 3.3 |
| Skin and Appendages | ||
| Rash | 4.9 | 4.5 |
| Sweating | 2.2 | 1.7 |
Laboratory Findings
Serum Calcium — Teriparatide transiently increased serum calcium, with the maximal effect observed at approximately 4 to 6 hours post-dose. Serum calcium measured at least 16 hours post-dose was not different from pretreatment levels. In clinical trials, the frequency of at least 1 episode of transient hypercalcemia in the 4 to 6 hours after teriparatide administration was increased from 2% of women and none of the men treated with placebo to 11% of women and 6% of men treated with teriparatide. The number of patients treated with teriparatide whose transient hypercalcemia was verified on consecutive measurements was 3% of women and 1% of men.
Urinary Calcium — Teriparatide increased urinary calcium excretion, but the frequency of hypercalciuria in clinical trials was similar for patients treated with teriparatide and placebo [see Clinical Pharmacology (12.2)].
Serum Uric Acid — Teriparatide increased serum uric acid concentrations. In clinical trials, 3% of teriparatide patients had serum uric acid concentrations above the upper limit of normal compared with 1% of placebo patients. However, the hyperuricemia did not result in an increase in gout, arthralgia, or urolithiasis.
Renal Function — No clinically important adverse renal effects were observed in clinical studies. Assessments included creatinine clearance; measurements of blood urea nitrogen (BUN), creatinine, and electrolytes in serum; urine specific gravity and pH; and examination of urine sediment.
Studies in Men and Women with Glucocorticoid-Induced Osteoporosis
The safety of teriparatide in the treatment of men and women with glucocorticoid-induced osteoporosis was assessed in a randomized, double-blind, active-controlled trial of 428 patients (19% men, 81% women) aged 22 to 89 years (mean 57 years) treated with ≥5 mg per day prednisone or equivalent for a minimum of 3 months. The duration of the trial was 18 months with 214 patients exposed to teriparatide and 214 patients exposed to oral daily bisphosphonate (active control). All patients received 1000 mg of calcium plus 800 IU of vitamin D supplementation per day.
The incidence of all cause mortality was 4% in the teriparatide group and 6% in the active control group. The incidence of serious adverse events was 21% in teriparatide patients and 18% in active control patients, and included pneumonia (3% teriparatide, 1% active control). Early discontinuation because of adverse events occurred in 15% of teriparatide patients and 12% of active control patients, and included dizziness (2% teriparatide, 0% active control).
Adverse events reported at a higher incidence in the teriparatide group and with at least a 2% difference in teriparatide-treated patients compared with active control-treated patients were: nausea (14%, 7%), gastritis (7%, 3%), pneumonia (6%, 3%), dyspnea (6%, 3%), insomnia (5%, 1%), anxiety (4%, 1%), and herpes zoster (3%, 1%), respectively.
Overdose Management — There is no specific antidote for teriparatide. Treatment of suspected overdose should include discontinuation of teriparatide injection, monitoring of serum calcium and phosphorus, and implementation of appropriate supportive measures, such as hydration.
The pharmacokinetic parameters of teriparatide following single subcutaneous administration of teriparatide injection in patients with osteoporosis are shown in Table 2.
| Mean ± S.D. | n | |
| Tmax (hr)* | 0.25 (0.12, 1.08) | 83 |
| Cmax (pg/mL) | 109.5 ± 62.8 | 83 |
| AUC0-t (pg·hr/mL) | 134.8 ± 79.7 | 83 |
| AUC0-inf (pg·hr/mL) | 149.8 ± 68.1 | 72 |
| t1/2 (hour) | 0.79 ± 0.35 | 72 |
Arithmetic mean ± S.D.; *Tmax = median (minimum, maximum)
Absorption — Teriparatide is absorbed after subcutaneous injection; the absolute bioavailability is approximately 95% based on pooled data from 20-, 40-, and 80-mcg doses. The rates of absorption and elimination are rapid. The peptide reaches peak serum concentrations about 30 minutes after subcutaneous injection of a 20-mcg dose and declines to non-quantifiable concentrations within 3 hours.
Distribution — Systemic clearance of teriparatide (approximately 62 L/hr in women and 94 L/hr in men) exceeds the rate of normal liver plasma flow, consistent with both hepatic and extra-hepatic clearance. Volume of distribution, following intravenous injection, is approximately 0.12 L/kg. The half-life of teriparatide in serum is 5 minutes when administered by intravenous injection. The longer half-life following subcutaneous administration reflects the time required for absorption from the injection site.
Elimination
Metabolism and Excretion — No metabolism or excretion studies have been performed with teriparatide. However, the mechanisms of metabolism and elimination of PTH(1-34) and intact PTH have been extensively described in published literature. Peripheral metabolism of PTH is believed to occur by non-specific enzymatic mechanisms in the liver followed by excretion via the kidneys.
Specific Populations
Pediatric Patients — Pharmacokinetic data in pediatric patients are not available [see Warnings and Precautions (5.1)].
Geriatric Patients — No age-related differences in teriparatide pharmacokinetics were detected (range 31 to 85 years).
Gender — Although systemic exposure to teriparatide was approximately 20% to 30% lower in men than women, the recommended dose for both genders is 20 mcg/day.
Race —The influence of race has not been determined.
Renal Impairment — No pharmacokinetic differences were identified in 11 patients with mild or moderate renal impairment [creatinine clearance (CrCl) 30 to 72 mL/min] administered a single dose of teriparatide. In 5 patients with severe renal impairment (CrCl <30 mL/min), the AUC and T1/2 of teriparatide were increased by 73% and 77%, respectively. Maximum serum concentration of teriparatide was not increased. No studies have been performed in patients undergoing dialysis for chronic renal failure [see Use in Specific Populations (8.7)].
Hepatic Impairment — No studies have been performed in patients with hepatic impairment [see Use in Specific Populations (8.6)].
Drug Interaction Studies
No pharmacokinetic drug-drug interaction studies have been conducted with teriparatide.
Effect on Fracture Incidence
New Vertebral Fractures — Teriparatide, when taken with calcium and vitamin D and compared with calcium and vitamin D alone, reduced the risk of 1 or more new vertebral fractures from 14.3% of women in the placebo group to 5.0% in the teriparatide group. This difference was statistically significant (p <0.001); the absolute reduction in risk was 9.3% and the relative reduction was 65%. Teriparatide was effective in reducing the risk for vertebral fractures regardless of age, baseline rate of bone turnover, or baseline BMD (see Table 3).
a p≤0.001 compared with placebo. | ||||
| Percent of Women With Fracture | ||||
Teriparatide (N=444) | Placebo (N=448) | Absolute Risk Reduction (%, 95% CI) | Relative Risk Reduction (%, 95% CI) | |
| New fracture (≥1) | 5.0a | 14.3 | 9.3 (5.5-13.1) | 65 (45-78) |
| 1 fracture | 3.8 | 9.4 | ||
| 2 fractures | 0.9 | 2.9 | ||
| ≥3 fractures | 0.2 | 2.0 | ||
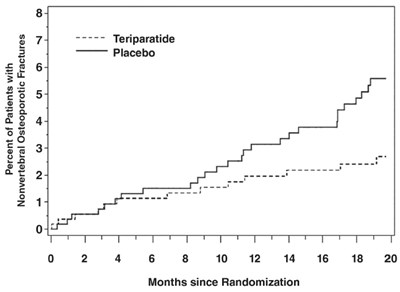
New Nonvertebral Osteoporotic Fractures — Teriparatide significantly reduced the risk of any nonvertebral fracture from 5.5% in the placebo group to 2.6% in the teriparatide group (p <0.05). The absolute reduction in risk was 2.9% and the relative reduction was 53%. The incidence of new nonvertebral fractures in the teriparatide group compared with the placebo group was ankle/foot (0.2%, 0.7%), hip (0.2%, 0.7%), humerus (0.4%, 0.4%), pelvis (0%, 0.6%), ribs (0.6%, 0.9%), wrist (0.4%, 1.3%), and other sites (1.1%, 1.5%), respectively.
The cumulative percentage of postmenopausal women with osteoporosis who sustained new nonvertebral fractures was lower in women treated with teriparatide than in women treated with placebo (see Figure 1).
Effect on Bone Mineral Density (BMD)
Teriparatide increased lumbar spine BMD in postmenopausal women with osteoporosis. Statistically significant increases were seen at 3 months and continued throughout the treatment period. Postmenopausal women with osteoporosis who were treated with teriparatide had statistically significant increases in BMD from baseline to endpoint at the lumbar spine, femoral neck, total hip, and total body (see Table 4).
a Intent-to-treat analysis, last observation carried forward. | ||
b p <0.001 compared with placebo. | ||
c p <0.05 compared with placebo. | ||
| Teriparatide N=541 | Placebo N=544 | |
| Lumbar spine BMD | 9.7b | 1.1 |
| Femoral neck BMD | 2.8c | -0.7 |
| Total hip BMD | 2.6c | -1.0 |
| Trochanter BMD | 3.5c | -0.2 |
| Intertrochanter BMD | 2.6c | -1.3 |
| Ward's triangle BMD | 4.2c | -0.8 |
| Total body BMD | 0.6c | -0.5 |
| Distal 1/3 radius BMD | -2.1 | -1.3 |
| Ultradistal radius BMD | -0.1 | -1.6 |
Teriparatide treatment increased lumbar spine BMD from baseline in 96% of postmenopausal women treated. Seventy-two percent of patients treated with teriparatide achieved at least a 5% increase in spine BMD, and 44% gained 10% or more.
Both treatment groups lost height during the trial. The mean decreases were 3.61 and 2.81 mm in the placebo and teriparatide groups, respectively.
Bone Histology
The effects of teriparatide on bone histology were evaluated in iliac crest biopsies of 35 postmenopausal women treated for 12 to 24 months with calcium and vitamin D and teriparatide 20 or 40 mcg/day. Normal mineralization was observed with no evidence of cellular toxicity. The new bone formed with teriparatide was of normal quality (as evidenced by the absence of woven bone and marrow fibrosis).
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of teriparatide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Osteosarcoma: Cases of bone tumor and osteosarcoma have been reported rarely in the postmarketing period. The causality to teriparatide use is unclear. Long term osteosarcoma surveillance studies are ongoing [see Warnings and Precautions (5.1)].
- Hypercalcemia: Hypercalcemia greater than 13.0 mg/dL has been reported with teriparatide use.
- Allergic Reactions: Anaphylactic reactions, drug hypersensitivity, angioedema, urticaria
- Investigations: Hyperuricemia
- Respiratory System: Acute dyspnea, chest pain
- Musculoskeletal: Muscle spasms of the leg or back
- Other: Injection site reactions including injection site pain, swelling and bruising; oro-facial edema
Adverse events reported since market introduction that were temporally (but not necessarily causally) related to teriparatide therapy include the following:
6.3 Immunogenicity
As with all peptides, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to teriparatide in the study described below with the incidence of antibodies in other studies or to other teriparatide products may be misleading.
The immunogenicity profile of teriparatide injection was evaluated in a 24-week randomized trial comparing the effects of teriparatide injection 20 mcg daily with another teriparatide product 20 mcg daily. In this trial, 2.2% (2/90) subjects who received teriparatide injection and 2.2% (2/91) subjects who received the other teriparatide product had detectable antibodies to teriparatide and one out of the two teriparatide injection treated patients developed neutralizing antibodies to teriparatide.
7.1 Digoxin
A single teriparatide dose did not alter the effect of digoxin on the systolic time interval (from electrocardiographic Q-wave onset to aortic valve closure, a measure of digoxin's calcium-mediated cardiac effect). However, because teriparatide may transiently increase serum calcium, teriparatide injection should be used with caution in patients taking digoxin [see Warnings and Precaution (5.8) and Clinical Pharmacology (12.2)].
7.2 Hydrochlorothiazide
The coadministration of hydrochlorothiazide 25 mg with teriparatide did not affect the serum calcium response to teriparatide 40 mcg. The effect of coadministration of a higher dose of hydrochlorothiazide with teriparatide on serum calcium levels has not been studied [see Clinical Pharmacology (12.2)].
7.3 Furosemide
Coadministration of intravenous furosemide (20 to 100 mg) with teriparatide 40 mcg in healthy people and patients with mild, moderate, or severe renal impairment (CrCl 13 to 72 mL/min) resulted in small increases in the serum calcium (2%) and 24-hour urine calcium (37%) responses to teriparatide that did not appear to be clinically important [see Clinical Pharmacology (12.2)].
8.1 Pregnancy
Risk Summary
There are no available data on teriparatide injection use in pregnant women to evaluate for drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Consider discontinuing teriparatide injection when pregnancy is recognized.
In animal reproduction studies, teriparatide increased skeletal deviations and variations in mouse offspring at subcutaneous doses equivalent to more than 60 times the recommended 20 mcg human daily dose (based on body surface area, mcg/m2), and produced mild growth retardation and reduced motor activity in rat offspring at subcutaneous doses equivalent to more than 120 times the human dose (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. The background risk in the US general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data
Animal Data
In animal reproduction studies, pregnant mice received teriparatide during organogenesis at subcutaneous doses 8 to 267 times the human dose (based on body surface area, mcg/m2). At doses ≥60 times the human dose, the fetuses showed an increased incidence of skeletal deviations or variations (interrupted rib, extra vertebra or rib). When pregnant rats received subcutaneous teriparatide during organogenesis at subcutaneous doses 16 to 540 times the human dose, the fetuses showed no abnormal findings.
In a perinatal/postnatal study in pregnant rats dosed subcutaneously from organogenesis through lactation, mild growth retardation was observed in female offspring at doses ≥120 times the human dose. Mild growth retardation in male offspring and reduced motor activity in both male and female offspring were observed at maternal doses of 540 times the human dose. There were no developmental or reproductive effects in mice or rats at doses 8 or 16 times the human dose, respectively.
8.2 Lactation
Risk Summary
It is not known whether teriparatide is excreted in human milk, affects human milk production, or has effects on the breast fed infant.
Because of the potential for osteosarcoma shown with teriparatide in animal studies, advise patients that breastfeeding is not recommended during treatment with teriparatide injection [see Warnings and Precautions (5.1)].
8.4 Pediatric Use
The safety and efficacy of teriparatide have not been established in any pediatric population. Teriparatide injection should not be prescribed in patients at an increased baseline risk of osteosarcoma which include pediatric and young adult patients with open epiphyses. Therefore, teriparatide injection is not indicated for use in pediatric or young adult patients with open epiphyses [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
Of the patients receiving teriparatide in the osteoporosis trial of 1637 postmenopausal women, 75% were 65 years of age and over and 23% were 75 years of age and over. Of the patients receiving teriparatide in the osteoporosis trial of 437 men, 39% were 65 years of age and over and 13% were 75 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
No studies have been performed in patients with hepatic impairment [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
In 5 patients with severe renal impairment (CrCl <30 mL/min), the AUC and T1/2 of teriparatide were increased by 73% and 77%, respectively. Maximum serum concentration of teriparatide was not increased [see Clinical Pharmacology (12.3)].
10 Overdosage
Incidents of overdose in humans have not been reported in clinical trials. Teriparatide has been administered in single doses of up to 100 mcg and in repeated doses of up to 60 mcg/day for 6 weeks. The effects of overdose that might be expected include a delayed hypercalcemic effect and risk of orthostatic hypotension. Nausea, vomiting, dizziness, and headache might also occur.
In postmarketing spontaneous reports, there have been cases of medication errors in which the entire contents (up to 800 mcg) of the teriparatide delivery device (pen) have been administered as a single dose. Transient events reported have included nausea, weakness/lethargy and hypotension. In some cases, no adverse events occurred as a result of the overdose. No fatalities associated with overdose have been reported.
11 Description
Teriparatide injection is a recombinant human parathyroid hormone analog (PTH 1-34). It has an identical sequence to the 34 N‑terminal amino acids (the biologically active region) of the 84-amino acid human parathyroid hormone.
The molecular formula of teriparatide is C181H291N55O51S2 and the molecular weight is 4117.8 daltons. Its amino acid sequence is shown below:
Teriparatide is manufactured using a strain of Pseudomonas fluorescens modified by recombinant DNA technology. Teriparatide injection is supplied as a sterile, colorless, clear, isotonic solution in a glass cartridge which is pre-assembled into a single-patient-use delivery device (pen) for subcutaneous injection. Each pen is filled to deliver 2.48 mL. Each mL contains 250 mcg teriparatide (as a free base), 0.41 mg glacial acetic acid, 0.10 mg sodium acetate, 45.4 mg mannitol, 3 mg metacresol, and water for injection. The drug product is a pH 4.0 solution.
Each cartridge, pre-assembled into a delivery device, delivers 20 mcg of teriparatide per dose each day for up to 28 days.
12.1 Mechanism Of Action
Endogenous 84-amino acid parathyroid hormone (PTH) is the primary regulator of calcium and phosphate metabolism in bone and kidney. Physiological actions of PTH include regulation of bone metabolism, renal tubular reabsorption of calcium and phosphate, and intestinal calcium absorption. The biological actions of PTH and teriparatide are mediated through binding to specific high-affinity cell-surface receptors. Teriparatide and the 34 N-terminal amino acids of PTH bind to these receptors with the same affinity and have the same physiological actions on bone and kidney. Teriparatide is not expected to accumulate in bone or other tissues.
The skeletal effects of teriparatide depend upon the pattern of systemic exposure. Once-daily administration of teriparatide stimulates new bone formation on trabecular and cortical (periosteal and/or endosteal) bone surfaces by preferential stimulation of osteoblastic activity over osteoclastic activity. In monkey studies, teriparatide improved trabecular microarchitecture and increased bone mass and strength by stimulating new bone formation in both cancellous and cortical bone. In humans, the anabolic effects of teriparatide manifest as an increase in skeletal mass, an increase in markers of bone formation and resorption, and an increase in bone strength. By contrast, continuous excess of endogenous PTH, as occurs in hyperparathyroidism, may be detrimental to the skeleton because bone resorption may be stimulated more than bone formation.
12.2 Pharmacodynamics
Pharmacodynamics in Men and Postmenopausal Women with Osteoporosis
Effects on Mineral Metabolism — Teriparatide affects calcium and phosphorus metabolism in a pattern consistent with the known actions of endogenous PTH (e.g., increases serum calcium and decreases serum phosphorus).
Serum Calcium Concentrations — When teriparatide 20 mcg is administered once daily, the serum calcium concentration increases transiently, beginning approximately 2 hours after dosing and reaching a maximum concentration between 4 and 6 hours (median increase, 0.4 mg/dL). The serum calcium concentration begins to decline approximately 6 hours after dosing and returns to baseline by 16 to 24 hours after each dose.
In a clinical study of postmenopausal women with osteoporosis, the median peak serum calcium concentration measured 4 to 6 hours after dosing with teriparatide (teriparatide 20 mcg) was 2.42 mmol/L (9.68 mg/dL) at 12 months. The peak serum calcium remained below 2.76 mmol/L (11.0 mg/dL) in >99% of women at each visit. Sustained hypercalcemia was not observed.
In this study, 11.1% of women treated with teriparatide had at least 1 serum calcium value above the upper limit of normal [2.64 mmol/L (10.6 mg/dL)] compared with 1.5% of women treated with placebo. The percentage of women treated with teriparatide whose serum calcium was above the upper limit of normal on consecutive 4- to 6-hour post-dose measurements was 3.0% compared with 0.2% of women treated with placebo. In these women, calcium supplements and/or teriparatide doses were reduced. The timing of these dose reductions was at the discretion of the investigator. Teriparatide dose adjustments were made at varying intervals after the first observation of increased serum calcium (median 21 weeks). During these intervals, there was no evidence of progressive increases in serum calcium.
In a clinical study of men with either primary or hypogonadal osteoporosis, the effects on serum calcium were similar to those observed in postmenopausal women. The median peak serum calcium concentration measured 4 to 6 hours after dosing with teriparatide was 2.35 mmol/L (9.44 mg/dL) at 12 months. The peak serum calcium remained below 2.76 mmol/L (11.0 mg/dL) in 98% of men at each visit. Sustained hypercalcemia was not observed.
In this study, 6.0% of men treated with teriparatide daily had at least 1 serum calcium value above the upper limit of normal [2.64 mmol/L (10.6 mg/dL)] compared with none of the men treated with placebo. The percentage of men treated with teriparatide whose serum calcium was above the upper limit of normal on consecutive measurements was 1.3% (2 men) compared with none of the men treated with placebo. Although calcium supplements and/or teriparatide doses could have been reduced in these men, only calcium supplementation was reduced [see Warnings and Precautions (5.5) and Adverse Reactions (6.1)].
In a clinical study of women previously treated for 18 to 39 months with raloxifene (n=26) or alendronate (n=33), mean serum calcium >12 hours after teriparatide injection was increased by 0.09 to 0.14 mmol/L (0.36 to 0.56 mg/dL), after 1 to 6 months of teriparatide treatment compared with baseline. Of the women pretreated with raloxifene, 3 (11.5%) had a serum calcium >2.76 mmol/L (11.0 mg/dL), and of those pretreated with alendronate, 3 (9.1%) had a serum calcium >2.76 mmol/L (11.0 mg/dL). The highest serum calcium reported was 3.12 mmol/L (12.5 mg/dL). None of the women had symptoms of hypercalcemia. There were no placebo controls in this study.
In the study of patients with glucocorticoid-induced osteoporosis, the effects of teriparatide on serum calcium were similar to those observed in postmenopausal women with osteoporosis not taking glucocorticoids.
Urinary Calcium Excretion — In a clinical study of postmenopausal women with osteoporosis who received 1000 mg of supplemental calcium and at least 400 IU of vitamin D, daily teriparatide increased urinary calcium excretion. The median urinary excretion of calcium was 4.8 mmol/day (190 mg/day) at 6 months and 4.2 mmol/day (170 mg/day) at 12 months. These levels were 0.76 mmol/day (30 mg/day) and 0.3 mmol/day (12 mg/day) higher, respectively, than in women treated with placebo. The incidence of hypercalciuria (>7.5 mmol Ca/day or 300 mg/day) was similar in the women treated with teriparatide or placebo.
In a clinical study of men with either primary or hypogonadal osteoporosis who received 1000 mg of supplemental calcium and at least 400 IU of vitamin D, daily teriparatide had inconsistent effects on urinary calcium excretion. The median urinary excretion of calcium was 5.6 mmol/day (220 mg/day) at 1 month and 5.3 mmol/day (210 mg/day) at 6 months. These levels were 0.5 mmol/day (20 mg/day) higher and 0.2 mmol/day (8.0 mg/day) lower, respectively, than in men treated with placebo. The incidence of hypercalciuria (>7.5 mmol Ca/day or 300 mg/day) was similar in the men treated with teriparatide or placebo.
Phosphorus and Vitamin D — In single-dose studies, teriparatide produced transient phosphaturia and mild transient reductions in serum phosphorus concentration. However, hypophosphatemia (<0.74 mmol/L or 2.4 mg/dL) was not observed in clinical trials with teriparatide.
In clinical trials of daily teriparatide, the median serum concentration of 1,25-dihydroxyvitamin D was increased at 12 months by 19% in women and 14% in men, compared with baseline. In the placebo group, this concentration decreased by 2% in women and increased by 5% in men. The median serum 25-hydroxyvitamin D concentration at 12 months was decreased by 19% in women and 10% in men compared with baseline. In the placebo group, this concentration was unchanged in women and increased by 1% in men.
In the study of patients with glucocorticoid-induced osteoporosis, the effects of teriparatide on serum phosphorus were similar to those observed in postmenopausal women with osteoporosis not taking glucocorticoids.
Effects on Markers of Bone Turnover — Daily administration of teriparatide to men and postmenopausal women with osteoporosis in clinical studies stimulated bone formation, as shown by increases in the formation markers serum bone-specific alkaline phosphatase (BSAP) and procollagen I carboxy-terminal propeptide (PICP). Data on biochemical markers of bone turnover were available for the first 12 months of treatment. Peak concentrations of PICP at 1 month of treatment were approximately 41% above baseline, followed by a decline to near-baseline values by 12 months. BSAP concentrations increased by 1 month of treatment and continued to rise more slowly from 6 through 12 months. The maximum increases of BSAP were 45% above baseline in women and 23% in men. After discontinuation of therapy, BSAP concentrations returned toward baseline. The increases in formation markers were accompanied by secondary increases in the markers of bone resorption: urinary N-telopeptide (NTX) and urinary deoxypyridinoline (DPD), consistent with the physiological coupling of bone formation and resorption in skeletal remodeling. Changes in BSAP, NTX, and DPD were lower in men than in women, possibly because of lower systemic exposure to teriparatide in men.
In the study of patients with glucocorticoid-induced osteoporosis, the effects of teriparatide on serum markers of bone turnover were similar to those observed in postmenopausal women with osteoporosis not taking glucocorticoids.
Digoxin — In a study of 15 healthy people administered digoxin daily to steady state, a single teriparatide dose did not alter the effect of digoxin on the systolic time interval (from electrocardiographic Q-wave onset to aortic valve closure, a measure of digoxin's calcium-mediated cardiac effect). However, sporadic case reports have suggested that hypercalcemia may predispose patients to digitalis toxicity. Because teriparatide may transiently increase serum calcium, teriparatide injection should be used with caution in patients taking digoxin [see Drug Interactions (7.1)].
Hydrochlorothiazide — In a study of 20 healthy people, the coadministration of hydrochlorothiazide 25 mg with teriparatide did not affect the serum calcium response to teriparatide 40 mcg. The 24-hour urine excretion of calcium was reduced by a clinically unimportant amount (15%). The effect of coadministration of a higher dose of hydrochlorothiazide with teriparatide on serum calcium levels has not been studied [see Drug Interactions (7.2)].
Furosemide — In a study of 9 healthy people and 17 patients with mild, moderate, or severe renal impairment (CrCl 13 to 72 mL/min), coadministration of intravenous furosemide (20 to 100 mg) with teriparatide 40 mcg resulted in small increases in the serum calcium (2%) and 24-hour urine calcium (37%) responses to teriparatide that did not appear to be clinically important [see Drug Interactions (7.3)].
12.3 Pharmacokinetics
The pharmacokinetic parameters of teriparatide following single subcutaneous administration of teriparatide injection in patients with osteoporosis are shown in Table 2.
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Carcinogenesis — Two carcinogenicity bioassays were conducted in Fischer 344 rats. In the first study, male and female rats were given daily subcutaneous teriparatide injections of 5, 30, or 75 mcg/kg/day for 24 months from 2 months of age. These doses resulted in systemic exposures that were, respectively, 3, 20, and 60 times higher than the systemic exposure observed in humans following a subcutaneous dose of 20 mcg (based on AUC comparison). Teriparatide treatment resulted in a marked dose-related increase in the incidence of osteosarcoma, a rare malignant bone tumor, in both male and female rats. Osteosarcomas were observed at all doses and the incidence reached 40% to 50% in the high-dose groups. Teriparatide also caused a dose-related increase in osteoblastoma and osteoma in both sexes. No osteosarcomas, osteoblastomas or osteomas were observed in untreated control rats. The bone tumors in rats occurred in association with a large increase in bone mass and focal osteoblast hyperplasia.
The second 2-year study was carried out in order to determine the effect of treatment duration and animal age on the development of bone tumors. Female rats were treated for different periods between 2 and 26 months of age with subcutaneous doses of 5 and 30 mcg/kg (equivalent to 3 and 20 times the human exposure at the 20-mcg dose, based on AUC comparison). The study showed that the occurrence of osteosarcoma, osteoblastoma and osteoma was dependent upon dose and duration of exposure. Bone tumors were observed when immature 2-month old rats were treated with 30 mcg/kg/day for 24 months or with 5 or 30 mcg/kg/day for 6 months. Bone tumors were also observed when mature 6-month old rats were treated with 30 mcg/kg/day for 6 or 20 months. Tumors were not detected when mature 6-month old rats were treated with 5 mcg/kg/day for 6 or 20 months. The results did not demonstrate a difference in susceptibility to bone tumor formation, associated with teriparatide treatment, between mature and immature rats.
The relevance of these animal findings to humans is uncertain.
Mutagenesis — Teriparatide was not genotoxic in any of the following test systems: the Ames test for bacterial mutagenesis; the mouse lymphoma assay for mammalian cell mutation; the chromosomal aberration assay in Chinese hamster ovary cells, with and without metabolic activation; and the in vivo micronucleus test in mice.
Impairment of Fertility — No effects on fertility were observed in male and female rats given subcutaneous teriparatide doses of 30, 100, or 300 mcg/kg/day prior to mating and in females continuing through gestation Day 6 (16 to 160 times the human dose of 20 mcg based on surface area, mcg/m2).
13.2 Animal Toxicology And/Or Pharmacology
In single-dose rodent studies using subcutaneous injection of teriparatide, no mortality was seen in rats given doses of 1000 mcg/kg (540 times the human dose based on surface area, mcg/m2) or in mice given 10,000 mcg/kg (2700 times the human dose based on surface area, mcg/m2).
In a long-term study, skeletally mature ovariectomized female monkeys (N=30 per treatment group) were given either daily subcutaneous teriparatide injections of 5 mcg/kg or vehicle. Following the 18-month treatment period, the monkeys were removed from teriparatide treatment and were observed for an additional 3 years. The 5 mcg/kg dose resulted in systemic exposures that were approximately 6 times higher than the systemic exposure observed in humans following a subcutaneous dose of 20 mcg (based on AUC comparison). Bone tumors were not detected by radiographic or histologic evaluation in any monkey in the study.
14.1 Treatment Of Osteoporosis In Postmenopausal Women
The safety and efficacy of once-daily teriparatide, median exposure of 19 months, were examined in a double-blind, multicenter, placebo-controlled clinical study of 1637 postmenopausal women with osteoporosis (teriparatide 20 mcg, n=541).
All women received 1000 mg of calcium and at least 400 IU of vitamin D per day. Baseline and endpoint spinal radiographs were evaluated using the semiquantitative scoring. Ninety percent of the women in the study had 1 or more radiographically diagnosed vertebral fractures at baseline. The primary efficacy endpoint was the occurrence of new radiographically diagnosed vertebral fractures defined as changes in the height of previously undeformed vertebrae. Such fractures are not necessarily symptomatic.
14.2 Treatment To Increase Bone Mass In Men With Primary Or Hypogonadal Osteoporosis
The safety and efficacy of once-daily teriparatide, median exposure of 10 months, were examined in a double-blind, multicenter, placebo-controlled clinical study of 437 men with either primary (idiopathic) or hypogonadal osteoporosis (teriparatide 20 mcg, n=151). All men received 1000 mg of calcium and at least 400 IU of vitamin D per day. The primary efficacy endpoint was change in lumbar spine BMD.
Teriparatide increased lumbar spine BMD in men with primary or hypogonadal osteoporosis. Statistically significant increases were seen at 3 months and continued throughout the treatment period. Teriparatide was effective in increasing lumbar spine BMD regardless of age, baseline rate of bone turnover, and baseline BMD. The effects of teriparatide at additional skeletal sites are shown in Table 5.
Teriparatide treatment for a median of 10 months increased lumbar spine BMD from baseline in 94% of men treated. Fifty-three percent of patients treated with teriparatide achieved at least a 5% increase in spine BMD, and 14% gained 10% or more.
a Intent-to-treat analysis, last observation carried forward. | ||
b p <0.001 compared with placebo. | ||
c p <0.05 compared with placebo. | ||
| Teriparatide N=151 | Placebo N=147 | |
| Lumbar spine BMD | 5.9b | 0.5 |
| Femoral neck BMD | 1.5c | 0.3 |
| Total hip BMD | 1.2 | 0.5 |
| Trochanter BMD | 1.3 | 1.1 |
| Intertrochanter BMD | 1.2 | 0.6 |
| Ward's triangle BMD | 2.8 | 1.1 |
| Total body BMD | 0.4 | -0.4 |
| Distal 1/3 radius BMD | -0.5 | -0.2 |
| Ultradistal radius BMD | -0.5 | -0.3 |
14.3 Treatment Of Men And Women With Glucocorticoid-Induced Osteoporosis
The efficacy of teriparatide for treating glucocorticoid-induced osteoporosis was assessed in a randomized, double-blind, active-controlled trial of 428 patients (19% men, 81% women) aged 22 to 89 years (mean 57 years) treated with ≥5 mg/day prednisone or equivalent for a minimum of 3 months. The duration of the trial was 18 months with 214 patients exposed to teriparatide. In the teriparatide group, the baseline median glucocorticoid dose was 7.5 mg/day and the median duration of glucocorticoid use was 1.5 years. The mean (SD) baseline lumbar spine BMD was 0.85 ± 0.13 g/cm2 and lumbar spine BMD T-score was –2.5 ± 1 (number of standard deviations below the mean BMD value for healthy adults). A total of 30% of patients had prevalent vertebral fracture(s) and 43% had prior non-vertebral fracture(s). The patients had chronic rheumatologic, respiratory or other diseases that required sustained glucocorticoid therapy. All patients received 1000 mg of calcium plus 800 IU of vitamin D supplementation per day.
Because of differences in mechanism of action (anabolic vs. anti-resorptive) and lack of clarity regarding differences in BMD as an adequate predictor of fracture efficacy, data on the active comparator are not presented.
Effect on Bone Mineral Density (BMD)
In patients with glucocorticoid-induced osteoporosis, teriparatide increased lumbar spine BMD compared with baseline at 3 months through 18 months of treatment. In patients treated with teriparatide, the mean percent change in BMD from baseline to endpoint was 7.2% at the lumbar spine, 3.6% at the total hip, and 3.7% at the femoral neck (p<0.001 all sites). The relative treatment effects of teriparatide were consistent in subgroups defined by gender, age, geographic region, body mass index, underlying disease, prevalent vertebral fracture, baseline glucocorticoid dose, prior bisphosphonate use, and glucocorticoid discontinuation during trial.
16.1 How Supplied
Teriparatide injection is available as single-patient-use pens in the following package size:
- 620 mcg/2.48 mL (250 mcg/mL) NDC 47781-652-89.
16.2 Storage And Handling
- The teriparatide injection delivery device should be stored under refrigeration at 2°C to 8°C (36°F to 46°F) at all times.
- Recap the delivery device when not in use to protect the cartridge from physical damage and light.
- During the use period, time out of the refrigerator should be minimized; the dose may be delivered immediately following removal from the refrigerator.
- Do not freeze. Do not use teriparatide injection if it has been frozen.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and User Manual).
17.1 Potential Risk Of Osteosarcoma
Patients should be made aware that, in rats, teriparatide caused an increase in the incidence of osteosarcoma (a malignant bone tumor) that was dependent on dose and treatment duration.
17.2 Orthostatic Hypotension
Teriparatide injection should be administered initially under circumstances where the patient can immediately sit or lie down if symptoms occur. Patients should be instructed that if they feel lightheaded or have palpitations after the injection, they should sit or lie down until the symptoms resolve. If symptoms persist or worsen, patients should be instructed to consult a physician before continuing treatment [see Warnings and Precautions (5.7)].
17.3 Hypercalcemia
Although symptomatic hypercalcemia was not observed in clinical trials, physicians should instruct patients taking teriparatide injection to contact a healthcare provider if they develop persistent symptoms of hypercalcemia (e.g., nausea, vomiting, constipation, lethargy, muscle weakness).
17.4 Other Osteoporosis Treatment Modalities
Patients should be informed regarding the roles of supplemental calcium and/or vitamin D, weight-bearing exercise, and modification of certain behavioral factors such as cigarette smoking and/or alcohol consumption.
17.5 Use Of Delivery Device (Pen)
Patients and caregivers who administer teriparatide injection should be instructed on how to properly use the delivery device (refer to User Manual), properly dispose of needles, and be advised not to share their delivery device with other patients. The contents of the delivery device should NOT be transferred to a syringe.
Each teriparatide injection delivery device can be used for up to 28 days including the first injection from the delivery device. After the 28-day use period, discard the teriparatide injection delivery device, even if it still contains some unused solution.
17.6 Availability Of Medication Guide And User Manual
Patients should read the Medication Guide and delivery device (pen) User Manual before starting therapy with teriparatide injection and re-read them each time the prescription is renewed. Patients need to understand and follow the instructions in the teriparatide injection delivery device User Manual. Failure to do so may result in inaccurate dosing.
Spl Medguide
| Medication Guide Teriparatide [ter i par a tide] Injection |
| Read this Medication Guide before you start taking teriparatide injection and each time you get a refill. There may be new information. Also, read the User Manual that comes with the teriparatide injection device (pen) for information on how to use the device to inject your medicine the right way. This Medication Guide does not take the place of talking with your healthcare provider about your medical condition or your treatment. |
What is the most important information I should know about teriparatide injection?
|
What is teriparatide injection?
Teriparatide injection should not be used in children and young adults whose bones are still growing. |
| Who should not use teriparatide injection? Do not use teriparatide injection if you are allergic to any of the ingredients in teriparatide injection. See the end of this Medication Guide for a complete list of the ingredients in teriparatide injection. |
Before you take teriparatide injection, tell your healthcare provider if you:
Especially tell your doctor if you take medicines that contain digoxin (Digoxin∗, Lanoxicaps∗, Lanoxin∗). |
How should I use teriparatide injection?
|
| What are the possible side effects of teriparatide injection? Teriparatide injection can cause serious side effects, including:
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of teriparatide injection. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
How should I store teriparatide injection?
|
| General information about teriparatide injection Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use teriparatide injection for a condition for which it was not prescribed. Do not give teriparatide injection to other people, even if they have the same condition you have. This Medication Guide summarizes the most important information about teriparatide injection. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about teriparatide injection that is written for healthcare professionals. For more information, call Alvogen, Inc. at 1-866-770-3024. |
| What are the ingredients in teriparatide injection? Active ingredient: teriparatide Inactive ingredients: glacial acetic acid, sodium acetate, mannitol, metacresol, and water for injection. |
| What is Osteoporosis? Osteoporosis is a disease in which the bones become thin and weak, increasing the chance of having a broken bone. Osteoporosis usually causes no symptoms until a fracture happens. The most common fractures are in the spine (backbone). They can shorten height, even without causing pain. Over time, the spine can become curved or deformed and the body bent over. Fractures from osteoporosis can also happen in almost any bone in the body, for example, the wrist, rib, or hip. Once you have had a fracture, the chance for more fractures greatly increases. The following risk factors increase your chance of getting fractures from osteoporosis:
|
| *The brands listed are trademarks of their respective owners and are not trademarks of Alvogen, Inc. Manufactured for: Pfenex, Inc. San Diego, CA 92121 USA Distributed by: Alvogen, Inc. Morristown, NJ 07960 USA |
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: October 2019
PL652-03
Prepare For Injection
| 1. Prepare Site and Remove the White Cap A) Wash hands prior to use. B) Prepare the injection site (thigh or abdomen) as recommended by your healthcare provider. C) Remove the white cap by pulling it straight off of the device (Figure B). |
| 2. Check Device, Device Label and Medication A) Check the device. DO NOT use the teriparatide injection device if it is damaged. B) Check the label on the device. DO NOT use if the device contains the incorrect medication or if the medication has expired (Figure C). C) Check the medication cartridge. The liquid medication should be clear and colorless. DO NOT use the medication if it is cloudy, colored, or has floating particles. (Figure C). |
| 3. Attach New Needle A) Peel off the paper tab (Figure D). B) Push the needle straight onto medicine cartridge. Screw on needle clockwise until firmly attached (Figure E and Figure F). DO NOT over-tighten the needle. |
| 4. Remove Outer Needle Cover Pull off large outer needle cover (Figure G), and save it for later (see Step 9). |
| 5. Set Dose Pull out the black injection button until it stops (Figure H). Check to make sure red stripe shows. Additionally, the instruction window will show an arrow pointing towards the needle end of the device (Figure I). |
| Troubleshooting If the device does not set fully or if you cannot pull back on the black injection button refer to Troubleshooting Problem E on the back page. |
Administer Injection
| 6. Remove Inner Needle Cover A) Pull off small inner needle protector and throw it away (Figure J). B) CAUTION: The needle will be exposed. |
| 7. Inject Dose A) Gently hold a fold of skin on your thigh or abdomen and insert the needle straight into the folded skin (Figure K). B) Press the black injection button down until it stops and hold (Figure L). C) Hold it in and count to 5 slowly. You must wait until the count of 5 to make sure the full dose has been delivered (Figure M). D) Remove the needle from the skin (Figure N). Once needle is removed from skin, take your thumb off the black injection button. |
| Note: You may not see the plunger moving. To confirm that your dose has been delivered, see Step 8. |
After Injection
| 8. Confirm Dose Check to make sure the black injection button is all the way down. The instruction window will show an arrow pointing towards the black button. If the yellow shaft does not show, you have finished the injection steps the right way (Figure O). |
| Important You should not see any of the yellow shaft. If you do and have already injected the medicine, do not inject yourself a second time in the same day. Instead, you must reset the device. Refer to Troubleshooting Problem A on the back page for more information. |
| 9. Remove Needle and Dispose A) Put the large outer needle cover on the needle by scooping it up and pressing it on (Figure P and Figure Q). Do not try to put the needle cover back on with your hands. B) Unscrew the covered needle all the way by giving the large needle cover 3-5 counter-clockwise turns (Figure R). Pull the needle straight off (Figure S). C) Dispose of the needle into a puncture resistant container according to local regulations (Figure T). DO NOT reuse needle. |
| Disposal Information For more information about how to correctly dispose of the needle refer to the Disposal Information section on the back page. |
| 10. Recap Device and Store A) Push white cap back on (Figure U). B) Always store the device in the refrigerator with the white cap on right after use (Figure V). DO NOT store the device with a needle attached. |
Troubleshooting
| Problem | Solution |
| A. The yellow shaft is still showing after I push in the black injection button. How do I reset my teriparatide injection delivery device? | To reset the teriparatide injection delivery device, follow the steps below: 1) If you have already injected, DO NOT inject yourself a second time on the same day. 2) Remove the needle and dispose in a sharps container according to local regulations. 3) Attach a new needle, pull off the large needle cover and save it. 4) Pull off the inner needle cover and throw away. 5) Point the needle down into an empty container. Push in the black injection button until it stops. Hold it in and slowly count to five. You may see a small stream or a drop of fluid. When you have finished, the black injection button should be all the way in. 6) If you still see the yellow shaft showing, contact Alvogen, Inc. (see Contact Information below and to the right) or your healthcare provider. 7) Remove the needle and dispose in a sharps container according to local regulations. Push the white cap back on, and put your teriparatide injection delivery device in the refrigerator. You can prevent this problem by always using a NEW needle for each injection, and by pushing the black injection button all the way in and slowly counting to five. |
| B. How can I tell if my teriparatide injection delivery device works? | The black injection button should be all the way in to show that the full dose of medicine has been injected from the teriparatide injection delivery device. Use a new needle every time you inject to be sure your teriparatide injection delivery device will work properly. |
| C. I see an air bubble in my teriparatide injection delivery device. | A small air bubble will not affect your dose and it will not harm you. You can continue to take your dose as usual. |
| D. I cannot get the needle off. | 1) Put the large needle cover on the needle. 2) Use the large needle cover to unscrew the needle. 3) Unscrew the needle all the way by giving the large needle cover 3 to 5 counter-clockwise turns. 4) If you still cannot get the needle off, ask someone to help you. |
| E. What should I do if I have difficulty pulling out the black injection button? | Change to a new teriparatide injection delivery device to take your dose as instructed by your healthcare provider. When the black injection button becomes hard to pull out, this means there is not enough medicine in your teriparatide injection delivery device for another dose. You may still see some medicine left in the cartridge. |
Disposal Information
Put your used needles in a FDA-cleared sharps disposal container right away after use.
DO NOT throw away (dispose of) loose needles in your household trash.
If you do not have a FDA-cleared sharps disposal container, you may use a container that is:
- Made of a heavy-duty plastic
- Can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out
- Upright and stable during use
- Leak-resistant
- Properly labeled to warn of hazardous waste inside the container
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles.
For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
DO NOT dispose of your used sharps disposal container in your household trash unless your community guidelines permit this.
DO NOT recycle your used sharps disposal container.
Cleaning And Storage
Cleaning Your Teriparatide Injection Delivery Device
- Wipe the outside of the teriparatide injection delivery device with a damp cloth.
- Do not place the teriparatide injection delivery device in water, or wash or clean it with any liquid.
- After each use, refrigerate the teriparatide injection delivery device right away. Read and follow the instructions in the Medication Guide section "How should I store teriparatide injection?".
- DO NOT store the teriparatide injection delivery device with a needle attached. Doing this may cause air bubbles to form in the medicine cartridge.
- Store the teriparatide injection delivery device with the white cap on.
- DO NOT freeze teriparatide injection. If the teriparatide injection delivery device has been frozen, throw the device away and use a new teriparatide injection delivery device. If the teriparatide injection delivery device has been left out of the refrigerator, do not throw the delivery device away. Place the delivery device back in the refrigerator and call Alvogen, Inc. (see Contact Information below).
Storing Your Teriparatide Injection Delivery Device
Other Important Notes
- The teriparatide injection delivery device contains 28 days of medicine.
- DO NOT transfer teriparatide injection to a syringe. This may result in you taking the wrong dose of medicine.
- Read and follow the instructions in the User Manual so that you use your teriparatide injection delivery device the right way.
- Check the teriparatide injection delivery device label to make sure you have the right medicine and that it has not expired.
- DO NOT use the teriparatide injection delivery device if it looks damaged. Look at the teriparatide injection medicine in the cartridge. If the medicine is not clear and colorless, or if it has particles, do not use it. Call Alvogen, Inc. if you notice any of these (see Contact Information below).
- Use a new needle for each injection.
- During injection, you may hear one or more clicks - this is normal.
- The teriparatide injection delivery device is not recommended for use by the blind or by those who have vision problems without help from a person trained in the proper use of the device.
- Keep your teriparatide injection delivery device and needles out of the reach of children.
Disposal Of Pen Needles And Delivery Device
Disposal of Pen Needles and the Teriparatide Injection Delivery Device
- Before throwing away the teriparatide injection delivery device, be sure to remove the pen needle.
- Throw away your teriparatide injection delivery device and used needles as instructed by your healthcare provider, local or state laws, or institutional policies.
| Dispose of the teriparatide injection delivery device 28 days after first use. | 1st Use Date: __________________ / __________________ / __________________ Throw Away After: __________________ / __________________ / __________________ |
Contact Information
If you have questions, need help or for more information with your teriparatide injection delivery device, contact Alvogen, Inc. at 1-866-770-3024 or your healthcare provider.
Manufactured for: Pfenex, Inc.
San Diego, CA 92121 USA
Distributed by: Alvogen, Inc.
Morristown, NJ 07960 USA
Revised: October 2019
IFU652-03
Package Label Principal Display Panel Section
NDC 47781-652-89
Rx only
Teriparatide Injection
620 mcg/2.48 mL (250 mcg/mL)
20 mcg per dose
For subcutaneous use
Do NOT transfer contents to a syringe.
Read User Manual BEFORE Injecting.
Each single-patient-use pen will deliver 28 subcutaneous doses.
Throw away 28 days after first use.
REFRIGERATE - DO NOT FREEZE
Do NOT transfer contents to a syringe.
NDC 47781-652-89
ATTENTION PHARMACIST: Medication Guide (attached to Prescribing Information) and device User Manual for patient inside carton.
Teriparatide Injection
620 mcg/2.48 mL (250 mcg/mL)
20 mcg per dose
Each single-patient-use pen will deliver 28 subcutaneous doses.
Date of first use ___/___/___
Discard unused portion 28 days after first use.
REFRIGERATE / DO NOT FREEZE
For subcutaneous use / Rx only
1 prefilled pen / Needles not included
Becton, Dickinson and Company pen needles from 29 to 31 gauge are recommended for use with this device
* Please review the disclaimer below.