FDA Label for Venlafaxine
View Indications, Usage & Precautions
- WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
- 1 INDICATIONS AND USAGE
- 2.1 IMPORTANT DOSING AND ADMINISTRATION INFORMATION
- 2.2 RECOMMENDED DOSAGE FOR THE TREATMENT OF MAJOR DEPRESSIVE DISORDER
- 2.3 RECOMMENDED DOSAGE FOR THE TREATMENT OF GENERALIZED ANXIETY DISORDER
- 2.4 SCREEN FOR BIPOLAR DISORDER PRIOR TO STARTING VENLAFAXINE EXTENDED-RELEASE TABLETS
- 2.5 SWITCHING PATIENTS FROM VENLAFAXINE TABLETS (IMMEDIATE-RELEASE FORMULATION)
- 2.6 DOSAGE RECOMMENDATIONS IN PATIENTS WITH HEPATIC IMPAIRMENT
- 2.7 DOSAGE RECOMMENDATIONS IN PATIENTS WITH RENAL IMPAIRMENT
- 2.8 DISCONTINUING TREATMENT WITH VENLAFAXINE EXTENDED-RELEASE TABLETS
- 2.9 SWITCHING PATIENTS TO OR FROM A MONOAMINE OXIDASE INHIBITOR (MAOI) ANTIDEPRESSANT
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5.1 SUICIDAL THOUGHTS AND BEHAVIORS IN ADOLESCENTS AND YOUNG ADULTS
- 5.2 SEROTONIN SYNDROME
- 5.3 ELEVATED BLOOD PRESSURE
- 5.4 INCREASED RISK OF BLEEDING
- 5.5 ANGLE-CLOSURE GLAUCOMA
- 5.6 ACTIVATION OF MANIA/HYPOMANIA
- 5.7 DISCONTINUATION SYNDROME
- 5.8 SEIZURES
- 5.9 HYPONATREMIA
- 5.10 WEIGHT AND HEIGHT CHANGES IN PEDIATRIC PATIENTS
- 5.11 APPETITE CHANGES IN PEDIATRIC PATIENTS
- 5.12 INTERSTITIAL LUNG DISEASE AND EOSINOPHILIC PNEUMONIA
- 5.13 SEXUAL DYSFUNCTION
- 6 ADVERSE REACTIONS
- 6.1 CLINICAL STUDIES EXPERIENCE
- 6.2 POSTMARKETING EXPERIENCE
- 7.1 DRUGS HAVING CLINICALLY IMPORTANT INTERACTIONS WITH VENLAFAXINE EXTENDED-RELEASE TABLETS
- 7.2 MONOAMINE OXIDASE INHIBITORS
- 8.1 PREGNANCY
- 8.2 LACTATION
- 8.4 PEDIATRIC USE
- 8.5 GERIATRIC USE
- 8.6 HEPATIC IMPAIRMENT
- 8.7 RENAL IMPAIRMENT
- 9.1 CONTROLLED SUBSTANCE
- 9.2 ABUSE
- 9.3 DEPENDENCE
- 10 OVERDOSAGE
- 11 DESCRIPTION
- 12.1 MECHANISM OF ACTION
- 12.2 PHARMACODYNAMICS
- 12.3 PHARMACOKINETICS
- 13.1 CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
- 14.1 MAJOR DEPRESSIVE DISORDER
- 14.2 GENERALIZED ANXIETY DISORDER
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- OTHER
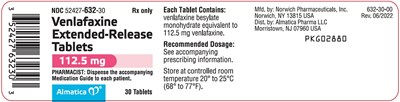
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL SECTION
Venlafaxine Product Label
The following document was submitted to the FDA by the labeler of this product Almatica Pharma Llc. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
Warning: Suicidal Thoughts And Behaviors
Antidepressants increased the risk of suicidal thoughts and behavior in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and emergence of suicidal thoughts and behaviors [see Warnings and Precautions (5.1)].
Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients[see Use in Specific Populations (8.4)].
1 Indications And Usage
Venlafaxine Extended-Release Tablets are indicated in adults for the treatment of:
- Major depressive disorder (MDD)
- Generalized Anxiety Disorder (GAD)
2.1 Important Dosing And Administration Information
Do not initiate venlafaxine treatment, titrate by doses less than 112.5 mg, or taper treatment with Venlafaxine Extended-Release Tablets, as dosing is not possible in these scenarios because Venlafaxine Extended-Release Tablets are only available in a 112.5 mg strength. Use another venlafaxine extended-release product for dosage initiation, titration, administration of dosages below 112.5 mg once daily, and to taper during discontinuation [see Dosage and Administration (2.6, 2.7, 2.8)]. Refer to the Prescribing Information of other venlafaxine extended-release products for the recommended dosage of those products in these dosing scenarios.
Venlafaxine Extended-Release Tablets can be initiated in patients who have received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days [see Dosage and Administration (2.2, 2.3)].
Administer Venlafaxine Extended-Release Tablets as once daily with food, either in the morning or in the evening at approximately the same time each day [see Clinical Pharmacology (12.3)]. Swallow tablets whole with fluid. Do not divide, crush, chew, or place in water.
2.2 Recommended Dosage For The Treatment Of Major Depressive Disorder
Initiate Venlafaxine Extended-Release Tablets at a dosage of 112.5 mg once daily in patients who have received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days [see Dosage and Administration (2.1)].
Patients not responding to their current venlafaxine dosage may benefit from dose increases to a maximum of 225 mg per day. Increase the dosage in increments of up to 75 mg per day, as needed, using another venlafaxine extended-release product at intervals of 4 days or more.
2.3 Recommended Dosage For The Treatment Of Generalized Anxiety Disorder
Initiate Venlafaxine Extended-Release Tablets at a dosage of 112.5 mg once daily in patients who have received at least 75 mg per day of another venlafaxine extended-release product for at least 4 days [see Dosage and Administration (2.1)].
Patients not responding to their current venlafaxine dosage may benefit from dose increases to a maximum of 225 mg per day. Increase the dosage in increments of up to 75 mg per day, as needed, using another venlafaxine extended-release product at intervals of 4 days or more.
2.4 Screen For Bipolar Disorder Prior To Starting Venlafaxine Extended-Release Tablets
Prior to initiating treatment with Venlafaxine Extended-Release Tablets, screen patients for a personal or family history of bipolar disorder, mania, or hypomania [see Warnings and Precautions (5.6)].
2.5 Switching Patients From Venlafaxine Tablets (Immediate-Release Formulation)
Patients who are currently receiving venlafaxine tablets (immediate-release formulation) may be switched to Venlafaxine Extended-Release Tablets at the nearest equivalent dose (mg per day) if the total daily dosage is either 112.5 mg or 225 mg once daily.
2.6 Dosage Recommendations In Patients With Hepatic Impairment
Reduce the total daily dose of venlafaxine by 50% in patients with mild (Child-Pugh Class A) to moderate (Child-Pugh Class B) hepatic impairment. In patients with severe hepatic impairment (Child-Pugh Class C) or hepatic cirrhosis, it may be necessary to reduce the dose by 50% or more [see Use in Specific Populations (8.6)].
The maximum recommended dosage of Venlafaxine Extended-Release Tablets in patients with hepatic impairment is 112.5 mg once daily. If the total daily dosage of venlafaxine is less than 112.5 mg per day, use another venlafaxine extended-release product [see Dosage and Administration (2.1)].
2.7 Dosage Recommendations In Patients With Renal Impairment
Reduce the total daily dose of venlafaxine by 25% to 50% in patients with mild (CLcr = 60-89 mL/min) or moderate (CLcr = 30-59 mL/min) renal impairment. In patients undergoing hemodialysis or with severe renal impairment (CLcr < 30 mL/min), the total daily dose should be reduced by 50% or more [see Use in Specific Populations (8.7)].
The maximum recommended dosage of Venlafaxine Extended-Release Tablets in patients with renal impairment is 112.5 mg once daily. If the total daily dosage of venlafaxine is less than 112.5 mg per day, use another venlafaxine extended-release product [see Dosage and Administration (2.1)].
2.8 Discontinuing Treatment With Venlafaxine Extended-Release Tablets
A gradual reduction in the dose, rather than abrupt cessation, is recommended whenever possible when discontinuing Venlafaxine Extended-Release Tablets. In clinical studies with venlafaxine extended-release capsules, tapering was achieved by reducing the daily dosage by 75 mg at one-week intervals.
Given that dosage strengths of Venlafaxine Extended-Release Tablets are not available below 112.5 mg, use another venlafaxine extended-release product for discontinuation [see Dosage and Administration (2.1)]. Individualization of tapering may be necessary. In some patients, discontinuation may need to occur over a period of several months [see Warnings and Precautions (5.7)].
2.9 Switching Patients To Or From A Monoamine Oxidase Inhibitor (Maoi) Antidepressant
At least 14 days must elapse between discontinuation of an MAOI (intended to treat psychiatric disorders) and initiation of therapy with Venlafaxine Extended-Release Tablets. In addition, at least 7 days should be allowed after stopping Venlafaxine Extended-Release Tablets before starting an MAOI intended to treat psychiatric disorders [see Contraindications (4), Warnings and Precautions (5.2), and Drug Interactions (7.1)].
3 Dosage Forms And Strengths
Extended-release tablets: 112.5 mg, white, round, biconvex tablet, with “ALM” over “632” printed in black ink on one side, and plain on the other side.
4 Contraindications
Venlafaxine Extended-Release Tablets are contraindicated in patients:
- with known hypersensitivity to venlafaxine besylate, venlafaxine hydrochloride, desvenlafaxine succinate or to any excipients in Venlafaxine Extended-Release Tablets [see Adverse Reactions (6.2)].
- taking, or within 14 days of stopping, MAOIs (including the MAOIs linezolid and intravenous methylene blue) because of increased risk of serotonin syndrome [see Dosage and Administration (2.9), Warnings and Precautions (5.2), Drug Interactions (7.1)].
5.1 Suicidal Thoughts And Behaviors In Adolescents And Young Adults
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients and 4,500 pediatric patients, the incidence of suicidal thoughts and behaviors in antidepressant-treated patients age 24 years and younger was greater than in placebo-treated patients. There was considerable variation in risk of suicidal thoughts and behaviors among drugs, but there was an increased risk identified in young patients for most drugs studied. There were differences in absolute risk of suicidal thoughts and behaviors across the different indications, with the highest incidence in patients with MDD. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1,000 patients treated are provided in Table 1.
| *Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients. | |
| Age Range | Drug-Placebo Difference in Number of Patients of Suicidal Thoughts and Behaviors per 1,000 Patients Treated |
| Increases Compared to Placebo | |
| < 18 years old | 14 additional patients |
| 18–24 years old | 5 additional patients |
| Decreases Compared to Placebo | |
| 25–64 years old | 1 fewer patient |
| ≥ 65 years old | 6 fewer patients |
It is unknown whether the risk of suicidal thoughts and behaviors in children, adolescents, and young adults extends to longer-term use, i.e., beyond four months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with MDD that antidepressants delay the recurrence of depression and that depression itself is a risk factor for suicidal thoughts and behaviors.
Monitor all antidepressant-treated patients for any indication for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy, and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing Venlafaxine Extended-Release Tablets, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
5.2 Serotonin Syndrome
Serotonin-norepinephrine reuptake inhibitors (SNRIs), including Venlafaxine Extended-Release Tablets, can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e., MAOIs [see Contraindications (4), Drug Interactions (7.1)]. Serotonin syndrome can also occur when these drugs are used alone.
Serotonin syndrome signs and symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of Venlafaxine Extended-Release Tablets with MAOIs is contraindicated. In addition, do not initiate Venlafaxine Extended-Release Tablets in a patient being treated with MAOIs such as linezolid or intravenous methylene blue. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection). If it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking Venlafaxine Extended-Release Tablets, discontinue Venlafaxine Extended-Release Tablets before initiating treatment with the MAOI [see Dosage and Administration (2.9), Contraindications (4), Drug Interactions (7.1)].
Monitor all patients taking Venlafaxine Extended-Release Tablets for the emergence of serotonin syndrome. Discontinue treatment with Venlafaxine Extended-Release Tablets and any concomitant serotonergic agents immediately if the above symptoms occur, and initiate supportive symptomatic treatment. If concomitant use of Venlafaxine Extended-Release Tablets with other serotonergic drugs is clinically warranted, inform patients of the increased risk for serotonin syndrome and monitor for symptoms.
5.3 Elevated Blood Pressure
In controlled trials, there were dose-related increases in systolic and diastolic blood pressure, as well as cases of sustained hypertension [see Adverse Reactions (6.1)].
Monitor blood pressure before initiating treatment with Venlafaxine Extended-Release Tablets and regularly during treatment. Control pre-existing hypertension before initiating treatment with Venlafaxine Extended-Release Tablets. Use caution in treating patients with pre-existing hypertension or cardiovascular or cerebrovascular conditions that might be compromised by increases in blood pressure. Sustained blood pressure elevation can lead to adverse outcomes. Cases of elevated blood pressure requiring immediate treatment have been reported with venlafaxine extended-release capsules. Consider dose reduction or discontinuation of treatment for patients who experience a sustained increase in blood pressure.
Across all clinical studies with venlafaxine, 1.4% of patients in the venlafaxine extended-release capsules treated groups experienced a ≥15 mm Hg increase in supine diastolic blood pressure (SDBP) ≥ 105 mm Hg, compared to 0.9% of patients in the placebo groups. Similarly, 1% of patients in the venlafaxine extended-release capsules treated groups experienced a ≥ 20 mm Hg increase in supine systolic blood pressure (SSBP) with blood pressure ≥ 180 mm Hg, compared to 0.3% of patients in the placebo groups [see Adverse Reactions (6.1)]. Treatment with venlafaxine extended-release capsules was associated with sustained hypertension (defined as SDBP ≥ 90 mm Hg and ≥ 10 mm Hg above baseline for three consecutive on-therapy visits) [see Adverse Reactions (6.1)]. An insufficient number of patients received mean doses of venlafaxine extended-release capsules over 300 mg per day in clinical studies to fully evaluate the incidence of sustained increases in blood pressure at these higher doses.
5.4 Increased Risk Of Bleeding
Drugs that interfere with serotonin reuptake inhibition, including Venlafaxine Extended-Release Tablets, may increase the risk of bleeding events, ranging from ecchymoses, hematomas, epistaxis, petechiae, and gastrointestinal hemorrhage to life-threatening hemorrhage. Concomitant use of aspirin, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), warfarin, and other anti-coagulants or other drugs known to affect platelet function may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Inform patients about the risk of bleeding associated with the concomitant use of Venlafaxine Extended-Release Tablets and antiplatelet agents or anticoagulants. For patients taking warfarin, carefully monitor coagulation indices when initiating, titrating, or discontinuing Venlafaxine Extended-Release Tablets.
5.5 Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs, including Venlafaxine Extended-Release Tablets, may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy. Avoid use of antidepressants, including Venlafaxine Extended-Release Tablets, in patients with untreated anatomically narrow angles.
5.6 Activation Of Mania/Hypomania
In patients with bipolar disorder, treating a depressive episode with Venlafaxine Extended-Release Tablets or another antidepressant may precipitate a mixed/manic episode. Mania or hypomania was reported in venlafaxine extended-release capsules treated patients in the premarketing studies in MDD (see Table 2). Prior to initiating treatment with Venlafaxine Extended-Release Tablets, screen for any personal or family history of bipolar, mania, or hypomania.
| Indication | Venlafaxine Extended-Release Capsules | Placebo |
|---|---|---|
| MDD | 0.3 | 0.0 |
| GAD | 0.0 | 0.2 |
5.7 Discontinuation Syndrome
Discontinuation symptoms have been systematically evaluated in patients taking venlafaxine, including prospective analyses of clinical studies in GAD and retrospective surveys of studies in MDD. Abrupt discontinuation or dose reduction of venlafaxine at various doses has been found to be associated with the appearance of new symptoms, the frequency of which increased with increased dose level and with longer duration of treatment. Reported symptoms include agitation, anorexia, anxiety, confusion, impaired coordination and balance, diarrhea, dizziness, dry mouth, dysphoric mood, fasciculation, fatigue, flu-like symptoms, headaches, hypomania, insomnia, nausea, nervousness, nightmares, sensory disturbances (including shock-like electrical sensations), somnolence, sweating, tremor, vertigo, and vomiting.
There have been postmarketing reports of serious discontinuation symptoms which can be protracted and severe. Completed suicide, suicidal thoughts, aggression and violent behavior have been observed in patients during reduction in venlafaxine extended-release capsules dosage, including during discontinuation. Other postmarketing reports describe visual changes (such as blurred vision or trouble focusing) and increased blood pressure after stopping or reducing the dose of venlafaxine extended-release capsules. During marketing of venlafaxine extended-release capsules, other SNRIs, and SSRIs, there have been reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: irritability, lethargy, emotional lability, tinnitus, and seizures.
Patients should be monitored for these symptoms when discontinuing treatment with Venlafaxine Extended-Release Tablets. A gradual reduction in the dose, rather than abrupt cessation, is recommended. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the healthcare provider may continue decreasing the dose, but at a more gradual rate. In some patients, discontinuation may need to occur over a period of several months [see Dosage and Administration (2.8)]. Given that dosage strengths of Venlafaxine Extended-Release Tablets are not available below 112.5 mg, use another venlafaxine extended-release product for discontinuation [see Dosage and Administration (2.1)].
5.8 Seizures
Cases of seizures have been reported with venlafaxine therapy. Venlafaxine Extended-Release Tablets has not been systematically evaluated in patients with seizure disorder. Venlafaxine Extended-Release Tablets should be prescribed with caution in patients with a history of seizures and should be discontinued in any patient who develops seizures.
5.9 Hyponatremia
Hyponatremia can occur as a result of treatment with SNRIs, including Venlafaxine Extended-Release Tablets In many cases, the hyponatremia appears to be the result of the Syndrome of Inappropriate Antidiuretic Hormone (SIADH) secretion. Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics, or those who are otherwise volume-depleted, may be at greater risk [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)]. Consider discontinuation of Venlafaxine Extended-Release Tablets in patients with symptomatic hyponatremia, and institute appropriate medical intervention.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.10 Weight And Height Changes In Pediatric Patients
Weight Changes
The average change in body weight and incidence of weight loss (percentage of patients who lost 3.5% or more) in the placebo-controlled pediatric studies in MDD and GAD with venlafaxine extended-release capsules are shown in Tables 3 and 4.
Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
| Indication (Study Duration) | Venlafaxine Extended-Release Capsules | Placebo |
|---|---|---|
| aVenlafaxine Extended-Release Tablets are not approved for use in pediatric patients. | ||
| MDD and GAD (4 pooled studies, 8 weeks) | -0.45 (n = 333) | +0.77 (n = 333) |
| Indication (Study Duration) | Venlafaxine Extended-Release Capsules | Placebo |
|---|---|---|
| a Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients. b p < 0.001 versus placebo | ||
| MDD and GAD (4 pooled studies, 8 weeks) | 18b (n = 333) | 3.6 (n = 333) |
Weight loss was not limited to patients with anorexia [see Warnings and Precautions (5.11)].
The risks associated with longer term use of venlafaxine extended-release capsules were assessed in an open-label MDD study of pediatric patients 6 years to 17 years old who received venlafaxine extended-release capsules for up to six months. The pediatric patients 6 years to 17 years old in the study had increases in weight that were less than expected, based on data from age- and sex-matched peers. The difference between observed weight gain and expected weight gain was larger for pediatric patients 6 years to < 12 years old than for pediatric patients ≥ 12 years old.
Height Changes
Table 5 shows the average height increase in pediatric patients in the short-term, placebo-controlled MDD and GAD studies with venlafaxine extended-release capsules. The differences in height increases in GAD and MDD studies were most notable in patients younger than twelve.
Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
| a Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients. b p = 0.041 | ||
| Indication (Study Duration) | Venlafaxine Extended-Release Capsules | Placebo |
| MDD (8 weeks) | 0.8 (n = 146) | 0.7 (n = 147) |
| GAD (8 weeks) | 0.3b (n = 122) | 1.0 (n = 132) |
In the six-month, open-label MDD study with venlafaxine extended-release capsules, pediatric patients 6 years to 17 years old had height increases that were less than expected, based on data from age- and sex-matched peers. The difference between observed and expected growth rates was larger for pediatric patients 6 years to < 12 years old than for pediatric patients ≥ 12 years old [see Use in Specific Populations (8.4)].
5.11 Appetite Changes In Pediatric Patients
Decreased appetite (reported as anorexia) was more commonly observed in venlafaxine extended-release capsule-treated pediatric patients 6 years to 17 years old versus placebo-treated patients in the premarketing evaluation of venlafaxine extended-release capsules for MDD and GAD (see Table 6).
Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
| Indication (Study Duration) | Venlafaxine Extended-Release Capsules Incidence | Discontinuation | Placebo Incidence | |
|---|---|---|---|---|
| a The discontinuation rates for weight loss were 0.7% for patients receiving either venlafaxine extended-release capsules or placebo. b Venlafaxine Extended-Release Tablets are not approved for use in pediatric patients. | ||||
| MDD and GAD (pooled, 8 weeks) | 10 | 0.0 | 3 | |
5.12 Interstitial Lung Disease And Eosinophilic Pneumonia
Interstitial lung disease and eosinophilic pneumonia associated with venlafaxine therapy have been rarely reported. The possibility of these events should be considered in Venlafaxine Extended-Release Tablets patients who present with progressive dyspnea, cough or chest discomfort. Such patients should undergo a prompt medical evaluation, and discontinuation of Venlafaxine Extended-Release Tablets should be considered.
5.13 Sexual Dysfunction
Use of SNRIs, including Venlafaxine Extended-Release Tablets, may cause symptoms of sexual dysfunction [see Adverse Reactions (6.1)]. In male patients, SNRI use may result in ejaculatory delay or failure, decreased libido, and erectile dysfunction. In female patients, SNRI use may result in decreased libido and delayed or absent orgasm.
It is important for prescribers to inquire about sexual function prior to initiation of Venlafaxine Extended-Release Tablets and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported. When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including the underlying psychiatric disorder. Discuss potential management strategies to support patients in making informed decisions about treatment.
6 Adverse Reactions
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Hypersensitivity [see Contraindications (4)]
- Suicidal Thoughts and Behaviors in Adolescents and Young Adults [see Warnings and Precautions (5.1)]
- Serotonin Syndrome [see Warnings and Precautions (5.2)]
- Elevated Blood Pressure [see Warnings and Precautions (5.3)]
- Increased Risk of Bleeding [see Warnings and Precautions (5.4)]
- Angle-Closure Glaucoma [see Warnings and Precautions (5.5)]
- Activation of Mania/Hypomania [see Warnings and Precautions (5.6)]
- Discontinuation Syndrome [see Warnings and Precautions (5.7)]
- Seizures [see Warnings and Precautions (5.8)]
- Hyponatremia [see Warnings and Precautions (5.9)]
- Weight and Height Changes in Pediatric Patients [see Warnings and Precautions (5.10)]
- Appetite Changes in Pediatric Patients [see Warnings and Precautions (5.11)]
- Interstitial Lung Disease and Eosinophilic Pneumonia [see Warnings and Precautions (5.12)]
- Sexual Dysfunction [see Warnings and Precautions (5.13)]
6.1 Clinical Studies Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
The safety of Venlafaxine Extended-Release Tabletsfor the treatment of MDD and GAD is based on adequate and well controlled studies of venlafaxine extended-release capsules. Below is a display of adverse reactions of venlafaxine extended-release capsules from those adequate and well-controlled studies in MDD, GAD, and other indications.
Most Common Adverse Reactions
The most commonly observed adverse reactions in the clinical study database in venlafaxine extended-release capsules treated patients in MDD, GAD, and other indications (incidence ≥ 5% and at least twice the rate of placebo) were: nausea (30.0%), somnolence (15.3%), dry mouth (14.8%), sweating (11.4%), abnormal ejaculation (9.9%), anorexia (9.8%), constipation (9.3%), impotence (5.3%) and decreased libido (5.1%).
Adverse Reactions Reported as Reasons for Discontinuation of Treatment
Combined across short-term, placebo-controlled premarketing studies for MDD, GAD, and other indications, 12% of the 3,558 patients who received venlafaxine extended-release capsules within a dosage range of 37.5 mg to 225 mg discontinued treatment due to an adverse reaction, compared with 4% of the 2,197 placebo-treated patients in those studies [Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength].
The most common adverse reactions leading to discontinuation in ≥ 1% of the venlafaxine extended-release capsules treated patients in the short-term studies (up to 12 weeks) in MDD, GAD, and other indications are shown in Table 7.
| Body System Adverse Reaction | Venlafaxine Extended-Release Capsules n = 3,558 | Placebo n = 2,197 |
Body as a whole | ||
Asthenia | 1.7 | 0.5 |
Headache | 1.5 | 0.8 |
Digestive system | ||
Nausea | 4.3 | 0.4 |
Nervous system | ||
Dizziness | 2.2 | 0.8 |
Insomnia | 2.1 | 0.6 |
Somnolence | 1.7 | 0.3 |
Skin and appendages | 1.5 | 0.6 |
Sweating | 1.0 | 0.2 |
Common Adverse Reactions in Placebo-controlled Studies
Common adverse reactions (those that occurred in ≥ 2% of venlafaxine extended-release capsules treated patients [357 MDD patients, 1,381 GAD patients, and 1,820 patients for other indications] and more frequently than placebo) in venlafaxine extended-release capsules treated patients in short-term, placebo-controlled, fixed- and flexible-dose clinical studies within a dosage range of doses 37.5 mg to 225 mg per day are shown in Table 8 [Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength].
The adverse reaction profile did not differ substantially between the different patient populations.
| a Percentages based on the number of men (venlafaxine extended-release capsules, n = 1,440; placebo, n = 923) b Percentages based on the number of women (venlafaxine extended-release capsules, n = 2,118; placebo, n = 1,274) | ||
| Body System Adverse Reaction | Venlafaxine Extended-Release Capsules n = 3,558 | Placebo n = 2,197 |
Body as a whole | ||
Asthenia | 12.6 | 7.8 |
Cardiovascular system | ||
Hypertension | 3.4 | 2.6 |
Palpitation | 2.2 | 2.0 |
Vasodilatation | 3.7 | 1.9 |
Digestive system | ||
Anorexia | 9.8 | 2.6 |
Constipation | 9.3 | 3.4 |
Diarrhea | 7.7 | 7.2 |
Dry mouth | 14.8 | 5.3 |
Nausea | 30.0 | 11.8 |
Vomiting | 4.3 | 2.7 |
Nervous system | ||
Abnormal dreams | 2.9 | 1.4 |
Dizziness | 15.8 | 9.5 |
Insomnia | 17.8 | 9.5 |
Libido decreased | 5.1 | 1.6 |
Nervousness | 7.1 | 5.0 |
Paresthesia | 2.4 | 1.4 |
Somnolence | 15.3 | 7.5 |
Tremor | 4.7 | 1.6 |
Respiratory system | ||
Yawn | 3.7 | 0.2 |
Skin and appendages | ||
Sweating (including night sweats) | 11.4 | 2.9 |
Special senses | ||
Abnormal vision | 4.2 | 1.6 |
Urogenital system | ||
Abnormal ejaculation/orgasm (men)a | 9.9 | 0.5 |
Anorgasmia (men)a | 3.6 | 0.1 |
Anorgasmia (women)b | 2.0 | 0.2 |
Impotence (men)a | 5.3 | 1.0 |
Other Adverse Reactions Observed in Clinical Studies
Body as a whole – Photosensitivity reaction, chills
Cardiovascular system – Postural hypotension, syncope, hypotension, tachycardia
Digestive system – Gastrointestinal hemorrhage [see Warnings and Precautions (5.4)], bruxism
Hemic/Lymphatic system – Ecchymosis [see Warnings and Precautions (5.4)]
Metabolic/Nutritional – Hypercholesterolemia, weight gain [see Warnings and Precautions (5.10)], weight loss [see Warnings and Precautions (5.10)]
Nervous system – Seizures [see Warnings and Precautions (5.8)], manic reaction [see Warnings and Precautions (5.6)], agitation, confusion, akathisia, hallucinations, hypertonia, myoclonus, depersonalization, apathy
Skin and appendages – Urticaria, pruritus, rash, alopecia
Special senses – Mydriasis, abnormality of accommodation, tinnitus, taste perversion
Urogenital system – Urinary retention, urination impaired, urinary incontinence, urinary frequency increased, menstrual disorders associated with increased bleeding or increased irregular bleeding (e.g., menorrhagia, metrorrhagia)
Vital Sign Changes
In placebo-controlled premarketing studies, there were increases in mean blood pressure (see Table 9). A dose-related increase in mean supine systolic and diastolic blood pressure was evident in patients treated with venlafaxine extended-release capsules. Across all clinical studies in MDD, GAD, and other indications, 1.4% of patients in the venlafaxine extended-release capsules groups experienced an increase in SDBP of ≥15 mm Hg along with a blood pressure ≥ 105 mm Hg, compared to 0.9% of patients in the placebo groups. Similarly, 1% of patients in the venlafaxine extended-release capsules groups experienced an increase in SSBP of ≥ 20 mm Hg with a blood pressure ≥ 180 mm Hg, compared to 0.3% of patients in the placebo groups.
| a Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength. b Maximum recommended dosage for Venlafaxine Extended-Release Tablets is 225 mg once daily. | ||||||
Venlafaxine Extended-Release Capsules | Placebo | |||||
Indication | ≤ 75 mg per daya | > 75 mg per daya,b | ||||
(Duration) | SSBP | SDBP | SSBP | SDBP | SSBP | SDBP |
MDD | ||||||
(8–12 weeks) | -0.28 | 0.37 | 2.93 | 3.56 | -1.08 | -0.10 |
GAD | ||||||
(8 weeks) | -0.28 | 0.02 | 2.40 | 1.68 | -1.26 | -0.92 |
(6 months) | 1.27 | -0.69 | 2.06 | 1.28 | -1.29 | -0.74 |
Venlafaxine extended-release capsules treatment was associated with sustained hypertension (defined as Supine Diastolic Blood Pressure [SDBP] ≥ 90 mm Hg and ≥ 10 mm Hg above baseline for three consecutive on-therapy visits (see Table 10).
| a Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength. b Maximum recommended dosage for Venlafaxine Extended-Release Tablets is 225 mg once daily. | ||
Indication | Dose Range (mg per day)a | Incidence (%) |
MDD | 75a to 375b | 19/705 (3) |
GAD | 37.5a to 225 | 5/1011 (0.5) |
Venlafaxine extended-release capsules was associated with mean increases in pulse rate compared with placebo in premarketing placebo-controlled studies (see Table 11) [see Warnings and Precautions (5.3, 5.4)].
Indication (Duration) | Venlafaxine Extended-Release Capsules | Placebo |
MDD (12 weeks) | 2 | 1 |
GAD (8 weeks) | 2 | < 1 |
Laboratory Changes
Serum Cholesterol
Venlafaxine extended-release capsules was associated with mean final increases in serum cholesterol concentrations compared with mean final decreases for placebo in premarketing MDD and GAD clinical studies (Table 12).
Indication (Duration) | Venlafaxine Extended-Release Capsules | Placebo | |
MDD | |||
(12 weeks) | +1.5 | -7.4 | |
GAD | |||
(8 weeks) | +1.0 | -4.9 | |
(6 months) | +2.3 | -7.7 | |
Venlafaxine extended-release capsules treatment for up to 12 weeks in premarketing placebo-controlled trials for major depressive disorder was associated with a mean final on-therapy increase in serum cholesterol concentration of approximately 1.5 mg/dL compared with a mean final decrease of 7.4 mg/dL for placebo. Venlafaxine extended-release capsules treatment for up to 8 weeks and up to 6 months in premarketing placebo-controlled GAD trials was associated with mean final on-therapy increases in serum cholesterol concentration of approximately 1.0 mg/dL and 2.3 mg/dL, respectively while placebo subjects experienced mean final decreases of 4.9 mg/dL and 7.7 mg/dL, respectively.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of venlafaxine extended-release capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a whole – Anaphylaxis, angioedema
Cardiovascular system – QT prolongation, ventricular fibrillation, ventricular tachycardia (including torsade de pointes), takotsubo cardiomyopathy
Digestive system – Pancreatitis
Hemic/Lymphatic system – Mucous membrane bleeding [see Warnings and Precautions (5.4)], blood dyscrasias (including agranulocytosis, aplastic anemia, neutropenia and pancytopenia), prolonged bleeding time, thrombocytopenia
Metabolic/Nutritional – Hyponatremia [see Warnings and Precautions (5.9)], Syndrome of Inappropriate Antidiuretic Hormone (SIADH) secretion [see Warnings and Precautions (5.9)], abnormal liver function tests, hepatitis, prolactin increased
Musculoskeletal – Rhabdomyolysis
Nervous system – Neuroleptic Malignant Syndrome (NMS) [see Warnings and Precautions (5.2)], serotonergic syndrome [see Warnings and Precautions (5.2)], delirium, extrapyramidal reactions (including dystonia and dyskinesia), impaired coordination and balance, tardive dyskinesia
Respiratory system – Dyspnea, interstitial lung disease, pulmonary eosinophilia [see Warnings and Precautions (5.12)]
Skin and appendages – Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme
Special senses – Angle-closure glaucoma [see Warnings and Precautions (5.5)]
7.1 Drugs Having Clinically Important Interactions With Venlafaxine Extended-Release Tablets
| Monoamine Oxidase Inhibitors (MAOI) | |
| Clinical Impact | Concomitant use of SNRIs, including Venlafaxine Extended-Release Tablets, with MAOIs increases the risk of serotonin syndrome. |
| Intervention | Concomitant use of Venlafaxine Extended-Release Tablets is contraindicated in patients taking MAOIs, including MAOIs such as linezolid or intravenous methylene blue [see Dosage and Administration (2.9), Contraindications (4), and Warnings and Precautions (5.2)]. |
| Other Serotonergic Drugs | |
| Clinical Impact | Concomitant use of Venlafaxine Extended-Release Tablets with other serotonergic drugs increases the risk of serotonin syndrome. |
| Intervention | Monitor for symptoms of serotonin syndrome when Venlafaxine Extended-Release Tablets is used concomitantly with other drugs that may affect the serotonergic neurotransmitter systems. If serotonin syndrome occurs, consider discontinuation of Venlafaxine Extended-Release Tablets and/or concomitant serotonergic drugs [see Dosage and Administration (2.8), Warnings and Precautions (5.2)]. |
| Alcohol | |
| Clinical Impact | Based on an in vitro study, alcohol increases the release rate of Venlafaxine Extended-Release Tablets [see Clinical Pharmacology (12.3)]. |
| Intervention | Avoid concomitant use of alcohol during treatment with Venlafaxine Extended-Release Tablets. |
| Drugs that Interfere with Hemostasis | |
| Clinical Impact | Concomitant use of Venlafaxine Extended-Release Tablets with an antiplatelet or anticoagulant drug may potentiate the risk of bleeding. This may be due to the effect of venlafaxine on the release of serotonin by platelets. |
| Intervention | Closely monitor patients receiving an antiplatelet or anticoagulant drug for bleeding when Venlafaxine Extended-Release Tablets is initiated or discontinued [see Warnings and Precautions (5.4)]. |
| CYP3A Inhibitors | |
| Clinical Impact | Concomitant use of Venlafaxine Extended-Release Tablets with a CYP3A inhibitor increases the Cmax and AUC of venlafaxine and O-desmethylvenlafaxine (ODV) [see Clinical Pharmacology (12.3)], which may increase the risk of toxicity of venlafaxine. |
| Intervention | Consider reducing the dose of Venlafaxine Extended-Release Tablets. |
| CYP2D6 Substrates | |
| Clinical Impact | Concomitant use of Venlafaxine Extended-Release Tablets with a CYP2D6 substrate increases Cmax and AUC of the CYP2D6 substrate, which may increase the risk of toxicity of the CYP2D6 substrate [see Clinical Pharmacology (12.3)]. |
| Intervention | Consider reduction in dose of concomitant CYP2D6 substrates. |
7.2 Monoamine Oxidase Inhibitors
Weight Loss Agents
The safety and efficacy of venlafaxine therapy in combination with weight loss agents, including phentermine, have not been established. Coadministration of Venlafaxine Extended-Release Tablets and weight loss agents is not recommended. Venlafaxine Extended-Release Tablets are not indicated for weight loss alone or in combination with other products.
Laboratory Test Interference
False-positive urine immunoassay screening tests for phencyclidine (PCP) and amphetamine have been reported in patients taking venlafaxine. This is due to lack of specificity of the screening tests. False positive test results may be expected for several days following discontinuation of venlafaxine therapy. Confirmatory tests, such as gas chromatography/mass spectrometry, will distinguish venlafaxine from PCP and amphetamine.
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antidepressants, including Venlafaxine Extended-Release Tablets, during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or visiting online at https://womensmentalhealth.org/research/pregnancyregistry/antidepressants.
Risk Summary
Available data from published epidemiologic studies on venlafaxine use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse fetal outcomes (see Data). Available data from observational studies with venlafaxine have identified a potential increased risk for preeclampsia when used during mid to late pregnancy; exposure to SNRIs near delivery may increase the risk for postpartum hemorrhage (see Clinical Considerations). There are risks associated with untreated depression in pregnancy and poor neonatal adaptation in newborns exposure to SNRIs, including Venlafaxine Extended-Release Tablets, during pregnancy (see Clinical Considerations).
In animal studies, there was no evidence of malformations or fetotoxicity following administration of venlafaxine during organogenesis at doses up to 2.5 times (rat) or 4 times (rabbit) the maximum recommended human daily dose on a mg/m2 basis. Postnatal mortality and decreased pup weights were observed following venlafaxine administration to pregnant rats during gestation and lactation at 2.5 times (mg/m2) the maximum human daily dose.
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Women who discontinue antidepressants during pregnancy are more likely to experience a relapse of major depression than women who continue antidepressants. This finding is from a prospective, longitudinal study of 201 women with a history of major depression who were euthymic at the beginning of pregnancy. Consider the risk of untreated depression when discontinuing or changing treatment with antidepressant medication during pregnancy and postpartum.
Maternal Adverse Reactions
Exposure to venlafaxine in mid to late pregnancy may increase the risk for preeclampsia, and exposure to SNRIs near delivery may increase the risk for postpartum hemorrhage.
Fetal/Neonatal Adverse Reactions
Neonates exposed to SNRIs late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremors, jitteriness, irritability, and constant crying. These findings are consistent with either a direct toxic effect of SNRIs or possibly a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome [see Warnings and Precautions (5.2)]. Monitor neonates who were exposed to Venlafaxine Extended-Release Tablets in the third trimester of pregnancy for drug discontinuation syndrome.
Data
Human Data
Published epidemiological studies of pregnant women exposed to venlafaxine have not established an increase of major birth defects, miscarriage, or other adverse developmental outcomes. Methodological limitations may both fail to identify true findings and also identify findings that are not true.
Retrospective cohort studies based on claims data have shown an association between venlafaxine use and preeclampsia, compared to depressed women who did not take an antidepressant during pregnancy. One study that assessed venlafaxine exposure in the second trimester or first half of the third trimester and preeclampsia showed an increased risk compared to unexposed depressed women (adjusted (adj) RR 1.57, 95% confidence interval [CI] 1.29-1.91). Preeclampsia was observed at venlafaxine doses equal to or greater than 75 mg per day and a duration of treatment >30 days. Another study that assessed venlafaxine exposure in gestational weeks 10-20 and preeclampsia showed an increased risk at doses equal to or greater than 150 mg per day. Available data are limited by possible outcome misclassification and possible confounding due to depression severity and other confounders.
Retrospective cohort studies based on claims data have suggested an association between venlafaxine use near the time of delivery or through delivery and postpartum hemorrhage. One study showed an increased risk for postpartum hemorrhage when venlafaxine exposure occurred through delivery, compared to unexposed depressed women (adj RR 2.24 [95% CI 1.69-2.97]). There was no increased risk in women who were exposed to venlafaxine earlier in pregnancy. Limitations of this study include possible confounding due to depression severity and other confounders. Another study showed an increased risk for postpartum hemorrhage when SNRI exposure occurred for at least 15 days in the last month of pregnancy or through delivery, compared to unexposed women (adj RR 1.64-1.76). The results of this study may be confounded by the effects of depression.
Animal Data
Venlafaxine did not cause malformations in offspring of rats or rabbits given doses up to 2.5 times (rat) or 4 times (rabbit) the maximum recommended human daily dose on a mg/m2 basis. However, in rats, there was a decrease in pup weight, an increase in stillborn pups, and an increase in pup deaths during the first 5 days of lactation, when dosing began during pregnancy and continued until weaning. The cause of these deaths is not known. These effects occurred at 2.5 times (mg/m2) the maximum human daily dose. The no effect dose for rat pup mortality was 0.25 times the human dose on a mg/m2 basis.
When desvenlafaxine succinate, the major metabolite of venlafaxine, was administered orally to pregnant rats and rabbits during the period of organogenesis at doses up to 300 mg/kg/day and 75 mg/kg/day, respectively, no fetal malformations were observed. These doses were associated with a plasma exposure (AUC) 19 times (rats) and 0.5 times (rabbits) the AUC exposure at an adult human dose of 100 mg per day. However, fetal weights were decreased and skeletal ossification was delayed in rats in association with maternal toxicity at the highest dose, with an AUC exposure at the no-effect dose that is 4.5-times the AUC exposure at an adult human dose of 100 mg per day.
8.2 Lactation
Risk Summary
Data from published literature report the presence of venlafaxine and its active metabolite in human milk and have not shown adverse reactions in breastfed infants (see Data). There are no data on the effects of venlafaxine on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Venlafaxine Extended-Release Tablets and any potential adverse effects on the breastfed child from Venlafaxine Extended-Release Tablets or from the underlying maternal condition.
Data
In a lactation study conducted in 11 breastfeeding women (at a mean of 20.1 months post-partum) who were taking a mean daily dose of 194.3 mg of venlafaxine and in a lactation study conducted in 6 breastfeeding women who were taking a daily dose of 225 mg to 300 mg of venlafaxine (at a mean of 7 months post-partum), the estimated mean relative infant dose was 8.1 % and 6.4% based on the sum of venlafaxine and its major metabolite, desvenlafaxine. No adverse reactions were seen in the infants.
8.4 Pediatric Use
Safety and effectiveness of Venlafaxine Extended-Release Tablets in pediatric patients have not been established.
Two placebo-controlled trials in 766 pediatric patients with MDD and two placebo-controlled trials in 793 pediatric patients with GAD have been conducted with venlafaxine extended-release capsules, and the data were not sufficient to support use in pediatric patients.
In the studies conducted in pediatric patients ages 6 to 17 years, the occurrence of blood pressure and cholesterol increases was considered to be clinically relevant in pediatric patients and was similar to that observed in adult patients [see Warnings and Precautions (5.3), Adverse Reactions (6.1)]. The following adverse reactions were also observed in pediatric patients: abdominal pain, agitation, dyspepsia, ecchymosis, epistaxis, and myalgia.
Although no studies have been designed to primarily assess Venlafaxine Extended-Release Tablet’s impact on the growth, development, and maturation of children and adolescents, the studies that have been done suggest that venlafaxine extended-release capsules may adversely affect weight and height [see Warnings and Precautions (5.10)]. Decreased appetite and weight loss were observed in placebo-controlled studies of pediatric patients 6 to 17 years [see Warnings and Precautions (5.10, 5.11)].
In pediatric clinical studies, the adverse reaction, suicidal ideation, was observed. Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric patients [see Boxed Warning, Warnings and Precautions (5.1)].
8.5 Geriatric Use
The percentage of patients in clinical studies for venlafaxine extended-release capsules for MDD and GAD who were 65 years of age or older are shown in Table 14.
| Indication | Venlafaxine Extended-Release Capsules |
|---|---|
| * In addition, in the premarketing assessment of venlafaxine tablets, 12% (357/2,897) of patients were ≥ 65 years of age. | |
| MDD | 4 (14/357) |
| GAD | 6 (77/1,381) |
No overall differences in effectiveness or safety were observed between geriatric patients and younger patients, and other reported clinical experience generally has not identified differences in response between the elderly and younger patients. However, greater sensitivity of some older individuals cannot be ruled out. SSRIs and SNRIs, including Venlafaxine Extended-Release Tablets, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event [see Warnings and Precautions (5.9)].
The pharmacokinetics of venlafaxine and ODV are not substantially altered in the elderly [see Clinical Pharmacology (12.3)]. No dose adjustment is recommended for the elderly on the basis of age alone, although other clinical circumstances, some of which may be more common in the elderly, such as renal or hepatic impairment, may warrant a dose reduction [see Dosage and Administration (2.6, 2.7)].
8.6 Hepatic Impairment
Dosage reduction is recommended in patients with mild (Child-Pugh Class A), moderate (Child-Pugh Class B), and severe (Child-Pugh Class C) hepatic impairment or hepatic cirrhosis [see Dosage and Administration (2.6) and Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Dosage reduction is recommended in patients with mild (CLcr = 60-89 mL/min) or moderate (CLcr = 30-59 mL/min) renal impairment, and in patients undergoing hemodialysis or with severe renal impairment (CLcr < 30 mL/min) [see Dosage and Administration (2.7) and Clinical Pharmacology (12.3)].
9.1 Controlled Substance
Venlafaxine Extended-Release Tablets contains venlafaxine which is not a controlled substance.
9.2 Abuse
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects.
While venlafaxine has not been systematically studied in clinical studies for its potential for abuse, there was no indication of drug-seeking behavior in the clinical studies. However, it is not possible to predict on the basis of premarketing experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, providers should carefully evaluate patients for history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of venlafaxine (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
9.3 Dependence
Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug.
In vitro studies revealed that venlafaxine has virtually no affinity for opiate, benzodiazepine, phencyclidine (PCP), or N-methyl-D-aspartic acid (NMDA) receptors.
Venlafaxine was not found to have any significant CNS stimulant activity in rodents. In primate drug discrimination studies, venlafaxine showed no significant stimulant or depressant abuse liability.
Discontinuation effects have been reported in patients receiving venlafaxine [see Dosage and Administration (2.8) and Warnings and Precautions (5.7)].
10 Overdosage
Human Experience
During the premarketing evaluations of venlafaxine extended-release capsules and immediate-release venlafaxine tablets (for MDD), there were twenty reports of acute overdosage with immediate-release venlafaxine tablets (6 and 14 reports in venlafaxine extended-release capsules and immediate-release venlafaxine tablets patients, respectively), either alone or in combination with other drugs and/or alcohol.
Somnolence was the most commonly reported symptom. Among the other reported symptoms were paresthesia of all four limbs, moderate dizziness, nausea, numb hands and feet, and hot-cold spells 5 days after the overdose. In most cases, no signs or symptoms were associated with overdose. The majority of the reports involved ingestion in which the total dose of venlafaxine taken was estimated to be no more than several-fold higher than the usual therapeutic dose. One patient who ingested 2.75 g of venlafaxine was observed to have two generalized convulsions and a prolongation of QTc to 500 msec, compared with 405 msec at baseline. Mild sinus tachycardia was reported in two of the other patients.
Actions taken to treat the overdose included no treatment, hospitalization and symptomatic treatment, and hospitalization plus treatment with activated charcoal. All patients recovered.
In postmarketing experience, overdose with venlafaxine has occurred predominantly in combination with alcohol and/or other drugs. The most commonly reported events in overdosage include tachycardia, changes in level of consciousness (ranging from somnolence to coma), mydriasis, seizures, and vomiting. Electrocardiogram changes (e.g., prolongation of QT interval, bundle branch block, QRS prolongation), ventricular tachycardia, bradycardia, hypotension, rhabdomyolysis, vertigo, liver necrosis, serotonin syndrome, and death have been reported.
Published retrospective studies report that venlafaxine overdosage may be associated with an increased risk of fatal outcomes compared to that observed with SSRI antidepressant products, but lower than that for tricyclic antidepressants. Epidemiological studies have shown that venlafaxine-treated patients have a higher preexisting burden of suicide risk factors than SSRI-treated patients. The extent to which the finding of an increased risk of fatal outcomes can be attributed to the toxicity of venlafaxine in overdosage, as opposed to some characteristic(s) of venlafaxine-treated patients, is not clear. Prescriptions for Venlafaxine Extended-Release Tablets should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Management of Overdosage
No specific antidotes for Venlafaxine Extended-Release Tablets are known. In managing overdosage, consider the possibility of multiple drug involvement. Consider contacting a Poison Center (1 800-222-1222) or a medical toxicologist for overdosage management recommendations for Venlafaxine Extended-Release Tablets.
11 Description
Venlafaxine Extended-Release Tablets contains venlafaxine, an SNRI, present as venlafaxine besylate monohydrate salt.
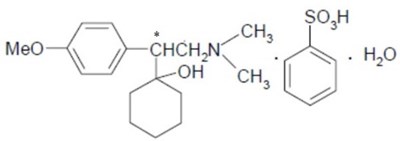
Venlafaxine besylate monohydrate is designated (R/S)-1-[2-(dimethylamino)-1-(4-methoxyphenyl)ethyl] cyclohexanol benzene sulfonate monohydrate or Cyclohexanol, 1-[2-(dimethylamino)-1-(4-methoxyphenyl)ethyl]-, benzenesulfonate, monohydrate and has the molecular formula of C23H33NO5S⸱H2O. Its molecular weight is 453.59. The structural formula is shown as follows:
Venlafaxine besylate is a white to almost white crystalline powder, with a solubility of about 32 mg/ml in water. Its octanol:water partition coefficient is 0.154.
Drug release is controlled by a combination of diffusion through the extended-release coating and erosion of the core tablets. The modified drug release is pH independent.
Venlafaxine Extended-Release Tablets are intended for oral administration and contains 183.95 mg of venlafaxine besylate monohydrate equivalent to 112.5 mg of venlafaxine.
Inactive ingredients: ammonio methacrylate copolymer, hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, povidone, silicon dioxide, simethicone, talc, titanium dioxide, and triacetin. The tablet printing ink is composed of ammonium hydroxide, black iron oxide, n-butyl alcohol, isopropyl alcohol, propylene glycol, and shellac.
12.1 Mechanism Of Action
The mechanism of action of venlafaxine in treatment of MDD and GAD is unclear, but is thought to be related to the potentiation of serotonin and norepinephrine in the central nervous system, through inhibition of reuptake of serotonin and norepinephrine.
12.2 Pharmacodynamics
In-Vitro studies have demonstrated that venlafaxine and its active metabolite, O-desmethylvenlafaxine (ODV), are potent and selective inhibitors of neuronal serotonin and norepinephrine reuptake and weak inhibitors of dopamine reuptake. Venlafaxine and ODV have no significant affinity for muscarinic-cholinergic, H1-histaminergic, or α1-adrenergic receptors in vitro. Pharmacologic activity at these receptors is hypothesized to be associated with the various anticholinergic, sedative, and cardiovascular effects seen with other psychotropic drugs. Venlafaxine and ODV do not possess monoamine oxidase (MAO) inhibitory activity.
12.3 Pharmacokinetics
Following single doses of Venlafaxine Extended-Release Tablets under fed conditions, the dose-normalized geometric mean area under curve (AUC) of venlafaxine and ODV were 93.21% and 93.14%, respectively, and the dose-normalized geometric mean peak concentration (Cmax) of venlafaxine and ODV were 93.27% and 106.3%, respectively, compared to those following venlafaxine extended-release capsules under fed conditions.
Steady-state plasma concentrations of venlafaxine and ODV are attained within 3 days of oral multiple-dose therapy.
Absorption
The absolute bioavailability of venlafaxine extended-release capsule is approximately 45%. Following a 112.5 mg Venlafaxine Extended-Release Tablets under fed conditions, the median time to attain Cmax (Tmax) was 10 hours (range 5-18 hours) for venlafaxine and 18 hours (range 5-28 hours) for ODV.
Effect of Food
Ingestion of a high-fat meal with Venlafaxine Extended-Release Tablets increases mean AUC of venlafaxine and ODV by 18% and 17%, respectively; increases mean Cmax of venlafaxine and ODV by 35% and 22%, respectively. Median Tmax was altered by food (median Tmax was 24 hours for both venlafaxine and ODV under fasted conditions).
Distribution
At therapeutic concentrations, venlafaxine and ODV are minimally bound to plasma proteins (27% and 30%, respectively). Administration of Venlafaxine Extended-Release Tablets to a patient taking another drug that is highly protein-bound should not cause increased free concentrations of the other drug. Following a single 112.5 mg dose of Venlafaxine Extended-Release Tablets, the mean apparent volume of distribution (Vz/F) of venlafaxine is 1375 L.
Elimination
Following a single 112.5 mg dose of Venlafaxine Extended-Release Tablets, the mean apparent clearance (CL/F) of venlafaxine is 170 L/hour and the mean elimination half-life (t1/2) of venlafaxine and ODV are 6.8 ± 1.6 hours and 11.3 ± 2.3 hours, respectively.
Metabolism
Following absorption, venlafaxine undergoes extensive pre-systemic metabolism in the liver, primarily to ODV, but also to N-desmethylvenlafaxine, N,O-didesmethylvenlafaxine, and other minor metabolites. In vitro studies indicate that the formation of ODV is catalyzed by CYP2D6; this has been confirmed in a clinical study showing that poor metabolizers of CYP2D6 had increased levels of venlafaxine and reduced levels of ODV compared to extensive metabolizers (Figure 1).
Excretion
Approximately 87% of a venlafaxine dose is recovered in the urine within 48 hours as unchanged venlafaxine (5%), unconjugated ODV (29%), conjugated ODV (26%), or other minor inactive metabolites (27%). Renal elimination of venlafaxine and its metabolites is the primary route of excretion.
Specific Population
A population pharmacokinetic analysis of patients from two studies receiving immediate-release venlafaxine tablets involving both twice daily and three times daily regimens showed that dose-normalized trough plasma levels of either venlafaxine or ODV were unaltered by age or gender differences.
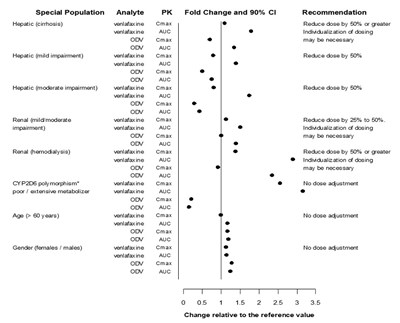
Exposures of venlafaxine and ODV in specific populations are summarized in Figure 1.
Figure 1: Pharmacokinetics of Venlafaxine and Active Metabolite O-Desmethylvenlafaxine (ODV) in Special Populations.
Abbreviations: ODV, O-desmethylvenlafaxine; AUC, area under the curve; Cmax, peak plasma concentrations; *Similar effect is expected with strong CYP2D6 inhibitors
Drug Interaction Studies
Effects of other drugs on the exposure of venlafaxine and ODV are summarized in Figure 2.
Figure 2: Effect of Interacting Drugs on the Pharmacokinetics of Venlafaxine and Active Metabolite O-desmethylvenlafaxine (ODV).
Abbreviations: ODV, O-desmethylvenlafaxine; AUC, area under the curve; Cmax, peak plasma concentrations; EM's, extensive metabolizers; PM's, poor metabolizers
* No dose adjustment on co-administration with CYP2D6 inhibitors.
Effects of venlafaxine on the exposure of other drugs are summarized in Figure 3.
Figure 3: Effect of Venlafaxine on the Pharmacokinetics of Interacting Drugs and Their Active Metabolites.
Abbreviations: AUC, area under the curve; Cmax, peak plasma concentrations; OH, hydroxyl
* Data for 2-OH desipramine were not plotted to enhance clarity; the fold change and 90% CI for Cmax and AUC of 2-OH desipramine were 6.6 (5.5, 7.9) and 4.4 (3.8, 5.0), respectively.
Alcohol: An in vitro study showed significant increase of venlafaxine release from Venlafaxine Extended-Release Tablets at 6 hours with approximately 100% of the drug release in the presence of 40% and 20% alcohol, respectively [see Drug Interactions (7.1)]. Effects of 5% and 10% alcohol on drug release were not significant compared to 0% alcohol. There is no in vivo study conducted for the effect of alcohol on drug exposure.
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Carcinogenesis
Tumors were not increased by venlafaxine treatment in mice or rats. Venlafaxine was given by oral gavage to mice for 18 months at doses up to 120 mg/kg per day, which was 1.7 times the maximum recommended human dose on a mg/m2 basis. Venlafaxine was also given to rats by oral gavage for 24 months at doses up to 120 mg/kg per day. In rats receiving the 120 mg/kg dose, plasma concentrations of venlafaxine at necropsy were 1 times (male rats) and 6 times (female rats) the plasma concentrations of patients receiving the maximum recommended human dose. Plasma levels of the ODV were lower in rats than in patients receiving the maximum recommended dose. ODV, the major human metabolite of venlafaxine, administered by oral gavage to mice and rats for 2 years did not increase the incidence of tumors in either study. Mice received ODV at dosages up to 500/300 mg/kg/day (dosage lowered after 45 weeks of dosing). The exposure at the 300 mg/kg/day dose is 9 times that of a human dose of 225 mg/day. Rats received ODV at dosages up to 300 mg/kg/day (males) or 500 mg/kg/day (females). The exposure at the highest dose is approximately 8 (males) or 11 (females) times that of a human dose of 225 mg/day.
Mutagenesis
Venlafaxine and the major human metabolite, ODV, were not mutagenic in the Ames reverse mutation assay in Salmonella bacteria or the Chinese hamster ovary/HGPRT mammalian cell forward gene mutation assay. Venlafaxine was also not mutagenic or clastogenic in the in vitro BALB/c-3T3 mouse cell transformation assay, the sister chromatid exchange assay in cultured Chinese hamster ovary cells, or in the in vivo chromosomal aberration assay in rat bone marrow. ODV was not clastogenic in the in vitro Chinese hamster ovary cell chromosomal aberration assay or in the in vivo chromosomal aberration assay in rats.
Impairment of Fertility
Reproduction and fertility studies of venlafaxine in rats showed no adverse effects of venlafaxine on male or female fertility at oral doses of up to 2 times the maximum recommended human dose of 225 mg/day on a mg/m2 basis. However, when desvenlafaxine succinate, the major human metabolite of venlafaxine, was administered orally to male and female rats, fertility was reduced at the high dose of 300 mg/kg/day, which is 10 (males) and 19 (females) times the AUC exposure at an adult human dose of 100 mg per day. There was no effect on fertility at 100 mg/kg/day, which is 3 (males) or 5 (females) times the AUC exposure at an adult human dose of 100 mg per day. These studies did not address reversibility of the effect on fertility. The relevance of these findings to humans is not known.
14.1 Major Depressive Disorder
The efficacy of Venlafaxine Extended-Release Tablets for the treatment of major depressive disorder (MDD) in adult patients is based upon adequate and well-controlled studies of venlafaxine extended-release capsules. The results of these adequate and well-controlled studies of venlafaxine extended-release capsules are presented below.
The efficacy of venlafaxine extended-release capsules as a treatment for Major Depressive Disorder (MDD) was established in two placebo-controlled, short-term (8 weeks for study 1; 12 weeks for study 2), flexible-dose studies, with doses starting at 75 mg per day and ranging to 225 mg per day in adult outpatients meeting DSM-III-R or DSM-IV criteria for MDD [Venlafaxine Extended-Release Tablets are only available in 112.5 mg dosage strength]. In moderately depressed outpatients, the initial dose of venlafaxine was 75 mg per day. In both studies, venlafaxine extended-release capsules demonstrated superiority over placebo on the primary efficacy measure defined as change from baseline in the HAM-D-21 total score to the endpoint visit. Venlafaxine extended-release capsules also demonstrated superiority over placebo on the key secondary efficacy endpoint, the Clinical Global Impressions (CGI) Severity of Illness scale. Examination of gender subsets of the population studied did not reveal any differential responsiveness on the basis of gender.
In a longer-term study, adult outpatients with MDD who had responded during an 8-week open-label study on venlafaxine extended-release capsules 75 mg, 150 mg, or 225 mg, once daily every morning were randomized to continuation of their same venlafaxine extended-release capsules dose or to placebo, for up to 26 weeks of observation for relapse. Response during the open-label phase was defined as a CGI Severity of Illness item score of ≤3 and a HAM-D-21 total score of ≤10 at the day 56 evaluation. Relapse during the double-blind phase was defined as follows: (1) a reappearance of major depressive disorder as defined by DSM-IV criteria and a CGI Severity of Illness item score of ≥4 (moderately ill), (2) 2 consecutive CGI Severity of Illness item scores of ≥4, or (3) a final CGI Severity of Illness item score of ≥4 for any patient who withdrew from the study for any reason. Patients receiving continued venlafaxine extended-release capsules treatment experienced statistically significantly lower relapse rates over the subsequent 26 weeks compared with those receiving placebo.
| Study number | Treatment Group | Primary Efficacy Measure: HAM-D Score | ||
|---|---|---|---|---|
| Mean Baseline Score (SD) | LS Mean Change from Baseline | Placebo Subtracted Differenceb (95%CI) | ||
| SD: standard deviation; LS Mean: least-squares mean; CI: confidence interval. a Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength. b Difference (drug minus placebo) in least-squares mean change from baseline. * Doses statistically significantly superior to placebo. | ||||
| Study 1 | Venlafaxine extended-release capsules (75 mga, 150 mga, 225 mg per day)* | 24.5 | -11.7 | -4.45 (-6.66,-2.25) |
| Placebo | 23.6 | -7.24 | - | |
| Study 2 | Venlafaxine extended-release capsules (75 mga, 150 mga, 225 mg per day)* | 24.5 | -15.11 | -6.40 (-8.45,-4.34) |
| Placebo | 24.9 | -8.71 | ||
14.2 Generalized Anxiety Disorder
The efficacy of Venlafaxine Extended-Release Tablets for the treatment of Generalized Anxiety Disorder (GAD) in adult patients is based upon adequate and well-controlled studies of venlafaxine extended-release capsules. The results of these adequate and well-controlled studies of venlafaxine extended-release capsules are presented below.
The efficacy of venlafaxine extended-release capsules as a treatment for Generalized Anxiety Disorder (GAD) was established in two 8-week, placebo-controlled, fixed-dose studies of 75 mg to 225 mg per day, one 6-month, placebo-controlled, flexible-dose study of 75 mg to 225 mg per day), and one 6-month, placebo-controlled, fixed-dose study of 37.5 mg, 75 mg, and 150 mg per day in adult outpatients meeting DSM-IV criteria for GAD [Venlafaxine Extended-Release Tablets are only available in 112.5 mg dosage strength].
In one 8-week study, venlafaxine extended-release capsules demonstrated superiority over placebo for the 75 mg, 150 mg, and 225 mg per day doses as measured by the Hamilton Rating Scale for Anxiety (HAM-A) total score, both the HAM-A anxiety and tension items, and the Clinical Global Impressions (CGI) scale. However, the 75 mg and 150 mg per day doses were not as consistently effective as the highest dose (Study 1). A second 8-week study evaluating doses of 75 mg and 150 mg per day and placebo showed that both doses were more effective than placebo on some of these same outcomes; however, the 75 mg per day dose was more consistently effective than the 150 mg per day dose (Study 2). A dose-response relationship for effectiveness in GAD was not clearly established in the 75 mg to 225 mg per day dose range studied.
Two 6-month studies, one evaluating venlafaxine extended-release capsules doses of 37.5 mg, 75 mg, and 150 mg per day (study 3) and the other evaluating venlafaxine extended-release capsules doses of 75 mg to 225 mg per day (study 4), showed that daily doses of 75 mg or higher were more effective than placebo on the HAM-A total, both the HAM-A anxiety and tension items, and the CGI scale during 6 months of treatment. While there was also evidence for superiority over placebo for the 37.5 mg per day dose, this dose was not as consistently effective as the higher doses.
Examination of gender subsets of the population studied did not reveal any differential responsiveness on the basis of gender.
| Study Number | Treatment Group | Primary Efficacy Measure: HAM-A Score | ||
|---|---|---|---|---|
| Mean Baseline Score (SD) | LS Mean Change from Baseline (SE)* | Placebo Subtracted Differenceb (95% CI) | ||
| SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval. a Venlafaxine Extended-Release Tablets are only available as 112.5 mg dosage strength. b Difference (drug minus placebo) in least-squares mean change from baseline. * Doses statistically significantly superior to placebo. | ||||
| Study 1 | Venlafaxine extended-release capsules 75 mga | 24.7 | -11.1 (0.95) | -1.5 (-3.8, 0.8) |
| 150 mga | 24.5 | -11.7 (0.87) | -2.2 (-4.5, 0.1) | |
| 225 mg | 23.6 | -12.1 (0.81) | -2.6 (-4.9, -0.3) | |
| Placebo | 24.1 | -9.5 (0.85) | ||
| Study 2 | Venlafaxine extended-release capsules 75 mga | 23.7 | -10.6 (0.82) | -2.6 (-4.6, -0.5) |
| 150 mga | 23.0 | -9.8 (0.86) | -1.7 (-3.8, 0.3) | |
| Placebo | 23.7 | -8.0 (0.73) | ||
| Study 3 | Venlafaxine extended-release capsules 37.5 mga | 26.6 (0.4) | -13.8 | -2.8 (-5.1, -0.6) |
| 75 mga | 26.3 (0.4) | -15.5 | -4.6 (-6.9, -2.3) | |
| 150 mga | 26.3 (0.4) | -16.4 | -5.5 (-7.8, -3.1) | |
| Placebo | 26.7 (0.5) | -11.0 | ||
| Study 4 | Venlafaxine extended-release capsules 75 mga to 225 mg | 25.0 | -13.4 (0.79) | - 4.7 (-6.6, -2.9) |
| Placebo | 24.9 | -8.7 (0.70) | ||
16 How Supplied/Storage And Handling
Venlafaxine Extended-Release Tablets are suppled as:
- 112.5 mg, white, round, biconvex tablet, with “ALM” over “632” printed in black ink on one side, and plain on the other side.
NDC 52427-632-30 Bottle of 30 tablets
Storage and Handling
Store at controlled room temperature 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Suicidal Thoughts and Behaviors
Advise patients, and caregivers to look for the emergence of suicidality especially early during treatment and when the dose is adjusted up or down, and instruct them to report such symptoms to the healthcare provider [see Boxed Warning and Warnings and Precautions (5.1)].
Concomitant Medication
Instruct patients not to take Venlafaxine Extended-Release Tablets with an MAOI or within 14 days of stopping an MAOI [see Contraindications (4)].
Serotonin Syndrome
Caution patients about the risk of serotonin syndrome, particularly with the concomitant use of Venlafaxine Extended-Release Tablets with other serotonergic drugs including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, amphetamines, tryptophan, buspirone, St. John’s Wort, and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid). Instruct patients to contact their health care provider or report to the emergency room if they experience signs or symptoms of serotonin syndrome [see Warnings and Precautions (5.2) and Drug Interactions (7.1)].
Elevated Blood Pressure
Advise patients that they should have regular monitoring of blood pressure when taking Venlafaxine Extended-Release Tablets [see Warnings and Precautions (5.3)].
Increased Risk of Bleeding
Inform patients about the concomitant use of Venlafaxine Extended-Release Tablets with NSAIDs, aspirin, other antiplatelet drugs, warfarin, or other drugs that affect coagulation because the combined use has been associated with an increased risk of bleeding. Advise patients to inform their health care providers if they are taking or planning to take any prescription or over-the-counter medications that increase the risk of bleeding [see Warnings and Precautions (5.4)].
Activation of Mania/Hypomania
Advise patients, their families and caregivers to observe for signs of activation of mania/hypomania and instruct them to report such symptoms to the healthcare provider [see Warnings and Precautions (5.6)].
Discontinuation Syndrome
Advise patients not to abruptly stop taking Venlafaxine Extended-Release Tablets without talking first with their healthcare provider. Patients should be aware that discontinuation effects may occur when stopping Venlafaxine Extended-Release Tablets and they should monitor for discontinuation symptoms [see Warnings and Precautions (5.7) and Adverse Reactions (6.1)].
Sexual Dysfunction
Advise patients that use of Venlafaxine Extended-Release Tablets may cause symptoms of sexual dysfunction in both male and female patients. Inform patients that they should discuss any changes in sexual function and potential management strategies with their healthcare provider [see Warnings and Precautions (5.13)].
Cardiovascular/Cerebrovascular Disease
Caution is advised in administering Venlafaxine Extended-Release Tablets to patients with cardiovascular, cerebrovascular, or lipid metabolism disorders [see Adverse Reactions (6.1)].
Serum Cholesterol and Triglyceride Elevation
Advise patients that elevations in total cholesterol, LDL and triglycerides may occur and that measurement of serum lipids may be considered [see Warnings and Precautions (6.1)].
Interference with Cognitive and Motor Performance
Caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that Venlafaxine Extended-Release Tablets therapy does not adversely affect their ability to engage in such activities.
Alcohol
Advise patients to avoid alcohol while taking Venlafaxine Extended-Release Tablets [see Drug Interactions (7.1)].
Allergic Reactions
Advise patients to notify their healthcare provider if they develop allergic phenomena such as rash, hives, swelling, or difficulty breathing [see Contraindications (4) and Adverse Reactions (6.2)].
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with Venlafaxine Extended-Release Tablets. Advise patients that Venlafaxine Extended-Release Tablets use during mid to late pregnancy may lead to an increased risk for preeclampsia; use in late pregnancy may lead to an increased risk for postpartum hemorrhage and may increase the risk for neonatal complications requiring prolonged hospitalization, respiratory support, and tube feeding. Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Venlafaxine Extended-Release Tablets during pregnancy [see Use in Specific Populations (8.1)].
Other
Manufactured by:
Norwich Pharmaceuticals, Inc.
Norwich, NY 13815 USA
Distributed by:
Almatica Pharma LLC
Morristown, NJ 07960 USA
PI632-00
Package Label Principal Display Panel Section
NDC 52427-632-30
Venlafaxine Extended-Release Tablets
112.5 mg
PHARMACIST: Dispense the accompanying Medication Guide to each patient.
Rx only
30 Tablets
* Please review the disclaimer below.