FDA Label for Amcinonide
View Indications, Usage & Precautions
- OTHER
- DESCRIPTION
- TOPICAL CREAM USP, 0.1%
- TOPICAL OINTMENT USP, 0.1%
- CLINICAL PHARMACOLOGY
- PHARMACOKINETICS
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
- GENERAL
- INFORMATION FOR THE PATIENT
- LABORATORY TESTS
- CARCINOGENESIS, MUTAGENESIS, AND IMPAIRMENT OF FERTILITY
- TERATOGENIC EFFECTS
- NURSING MOTHERS
- PEDIATRIC USE
- ADVERSE REACTIONS
- OVERDOSAGE
- DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- STORAGE AND HANDLING
- PRINCIPAL DISPLAY PANEL - 30 G TUBE CARTON
Amcinonide Product Label
The following document was submitted to the FDA by the labeler of this product Sun Pharmaceutical Industries, Inc.. The document includes published materials associated whith this product with the essential scientific information about this product as well as other prescribing information. Product labels may durg indications and usage, generic names, contraindications, active ingredients, strength dosage, routes of administration, appearance, warnings, inactive ingredients, etc.
Other
Rx only.
Mfd. By: Taro Pharmaceutical Industries Ltd., Haifa Bay, Israel 26110
Revised: February, 2010
90056-0210-5 291
Description
The topical corticosteroids constitute a class of primarily synthetic steroids used as anti-inflammatory and antipruritic agents.
Topical Cream Usp, 0.1%
Each gram of Amcinonide Cream contains 1 mg of the active steroid amcinonide in a white, smooth, homogeneous, opaque emulsion composed of benzyl alcohol (as preservative), emulsifying wax, glycerin, isopropyl palmitate, lactic acid, purified water and sorbitol solution 70%.
Topical Ointment Usp, 0.1%
Each gram of Amcinonide Ointment contains 1 mg of the active steroid amcinonide in a specially formulated base composed of benzyl alcohol 2.2% (wt/wt) as preservative, butylated hydroxyanisole, citric acid anhydrous, emulsifying wax, propyl gallate, propylene glycol, and white petrolatum.
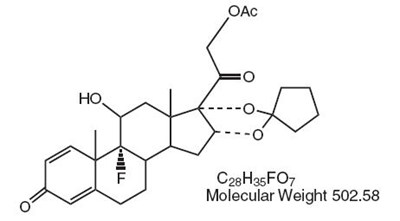
Chemically, amcinonide is:
Pregna-1,4-diene-3,20-dione, 21-(acetyloxy)-16,17-[cyclopentylidenebis (oxy)]-9-fluoro-11-hydroxy-, (11β, 16α).
Clinical Pharmacology
Topical corticosteroids share anti-inflammatory, antipruritic and vasoconstrictive actions.
The mechanism of anti-inflammatory activity of the topical corticosteroids is unclear. Various laboratory methods, including vasoconstrictor assays, are used to compare and predict potencies and/or clinical efficacies of the topical corticosteroids. There is some evidence to suggest that a recognizable correlation exists between vasoconstrictor potency and therapeutic efficacy in man.
Pharmacokinetics
The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings.
Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids (see DOSAGE AND ADMINISTRATION).
Once absorbed through the skin, topical corticosteroids are handled through pharmacokinetic pathways similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees.
Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted into the bile.
Indications And Usage
Topical corticosteroids are indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses.
Contraindications
Topical corticosteroids are contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
General
Systemic absorption of topical corticosteroids has produced reversible hypothalamic-pituitary-adrenal (HPA) axis suppression, manifestations of Cushing's syndrome, hyperglycemia and glucosuria in some patients.
Conditions that augment systemic absorption include the application of the more potent steroids, use over large surface areas, prolonged use and the addition of occlusive dressings. Therefore, patients receiving a large dose of a potent topical steroid applied to a large surface area or under an occlusive dressing should be evaluated periodically for evidence of HPA axis suppression by using the urinary free cortisol and ACTH stimulation tests. If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute with a less potent steroid.
Recovery of HPA axis function is generally prompt and complete upon discontinuation of the drug.
Infrequently, signs and symptoms of steroid withdrawal may occur, requiring supplemental systemic corticosteroids.
Pediatric patients may absorb proportionally larger amounts of topical corticosteroids and thus be more susceptible to systemic toxicity (see PRECAUTIONS Pediatric Use).
If irritation develops, topical corticosteroids should be discontinued and appropriate therapy instituted.
In the presence of dermatological infections, the use of an appropriate antifungal or antibacterial agent should be instituted. If a favorable response does not occur promptly, the corticosteroid should be discontinued until the infection has been adequately controlled.
These products are not for ophthalmic use.
Information For The Patient
Patients using topical corticosteroids should receive the following information and instructions:
- This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes.
- Patients should be advised not to use this medication for any disorder other than that for which it was prescribed.
- The treated skin area should not be bandaged or otherwise covered or wrapped as to be occlusive unless directed by the physician.
- Patients should report any signs of local adverse reactions especially under occlusive dressing.
- Parents of pediatric patients should be advised not to use tight-fitting diapers or plastic pants on a child being treated in the diaper area since these garments may constitute occlusive dressings.
Laboratory Tests
The following tests may be helpful in evaluating the HPA axis suppression:
Urinary free cortisol test
ACTH stimulation test
Carcinogenesis, Mutagenesis, And Impairment Of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential or the effect on fertility of topical corticosteroids.
Studies to determine mutagenicity with prednisolone and hydrocortisone have revealed negative results.
Teratogenic Effects
Corticosteroids are generally teratogenic in laboratory animals when administered systemically at relatively low dosage levels. The more potent corticosteroids have been shown to be teratogenic after dermal application in laboratory animals. There are no adequate and well-controlled studies in pregnant women on teratogenic effects from topically applied corticosteroids. Therefore, topical corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Drugs of this class should not be used extensively on pregnant patients, in large amounts, or for prolonged periods of time.
Nursing Mothers
It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in breast milk. Systemically administered corticosteroids are secreted into breast milk in quantities not likely to have a deleterious effect on the infant. Nevertheless, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Pediatric patients may demonstrate greater susceptibility to topical corticosteroid-induced HPA axis suppression and Cushing's syndrome than mature patients because of a larger skin surface area to body weight ratio.
Hypothalamic-pituitary-adrenal (HPA) axis suppression, Cushing's syndrome, and intracranial hypertension have been reported in pediatric patients receiving topical corticosteroids. Manifestations of adrenal suppression in pediatric patients include linear growth retardation, delayed weight gain, low plasma cortisol levels, and absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Administration of topical corticosteroids to pediatric patients should be limited to the least amount compatible with an effective therapeutic regimen. Chronic corticosteroid therapy may interfere with the growth and development of pediatric patients.
Adverse Reactions
The following local adverse reactions are reported infrequently with topical corticosteroids, but may occur more frequently with the use of occlusive dressings. These reactions are listed in an approximate decreasing order of occurrence:
Overdosage
Topically applied corticosteroids can be absorbed in sufficient amounts to produce systemic effects (see PRECAUTIONS).
Dosage And Administration
Topical corticosteroids are generally applied to the affected area as a thin film from two to three times daily depending on the severity of the condition.
Occlusive dressings may be a valuable therapeutic adjunct for the management of psoriasis or recalcitrant conditions.
If an infection develops, the use of occlusive dressings should be discontinued and appropriate antimicrobial therapy instituted.
How Supplied
Amcinonide Topical Cream USP, 0.1% (1 mg/g) is supplied in 4 gm, 15 gm, 30 gm and 60 gm tubes.
Amcinonide Topical Ointment USP, 0.1% (1 mg/g) is supplied in 15 gm, 30 gm and 60 gm tubes.
Storage And Handling
Store at 20° -25°C (68°-77°F) [see USP Controlled Room Temperature]
DO NOT FREEZE.
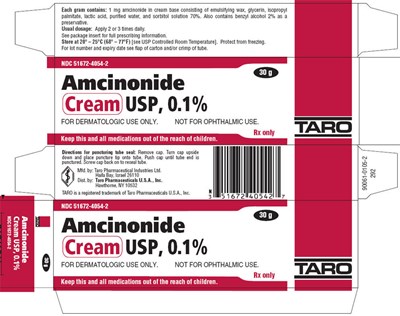
Principal Display Panel - 30 G Tube Carton
NDC 51672-4054-2
30 g
Amcinonide
Cream USP, 0.1%
FOR DERMATOLOGIC USE ONLY.
NOT FOR OPHTHALMIC USE.
Rx only
TARO
Keep this and all medications out of the reach of children.
NDC 51672-4060-2
30 g
Amcinonide
Ointment USP, 0.1%
FOR DERMATOLOGIC USE ONLY.
NOT FOR OPHTHALMIC USE.
Rx only
TARO
Keep this and all medications out of the reach of children.
* Please review the disclaimer below.